老年乳腺癌的发病率在逐年增加,流行病学提示美国≥60岁的乳腺癌患者占所有新发乳腺癌的比率≥50%[1]。在国内,2008年55~69岁妇女乳腺癌的发病率约60/10万,所有乳腺癌患者中≥65岁的患者占16.6%,预计到2030年≥65岁的患者将达27%[2]。老年乳腺癌患者多伴有重要器官功能衰退、全身伴随疾病多、对治疗耐受力差、术后辅助化疗的获益不明显[3]等特点,目前乳腺癌治疗策略的临床试验数据主要来源于年轻患者,有关老年乳腺癌的循证治疗依据很少,尚无对老年乳腺癌治疗的统一方案。国内外学术界对“老年乳腺癌”的定义很不一致,以≥65岁定义居多。本研究研究以≥65岁为老年乳腺癌的界限,老年乳腺癌患者的临床病理特点及预后进行回顾性分析,期望为老年乳腺癌的治疗提供参考依据。
1 资料与方法
1.1 临床资料
收集广东省妇幼保健院2003年1月1日~2012年12月31日73例Ⅰ~ⅢA期的乳腺癌患者的临床病理学资料,患者年龄65~84岁,中位年龄70岁。所有患者均接受手术治疗,并根据具体情况接受了辅助放化疗和内分泌治疗。进入分析的患者均具备完整的临床资料,包括一般情况、病理诊断、肿瘤分期、雌激素受体(estrogen receptor,ER)、孕激素受体(progesterone receptor,PR)、HER2、复发情况和生存状况等;同时具备较完整的随访资料,包括转移时间及其部位或死亡时间。
1.2 随访
采用门诊定期复查、信访和电话随访相结合的方式,随访至患者死亡或截止日期为2018年12月31日。预后评价指标为无病生存率(disease-free survival,DFS)和总生存率(overall survival,OS)。DFS的定义为从手术日期至发现肿瘤复发或转移(第一事件)的时间,OS的定义为从手术日期至死亡日期的时间。
1.3 统计学方法
应用SPSS 19.0软件进行统计学分析。临床、病理特征的组间比较使用卡方检验,生存率分析采用Kaplan-Meier方法,Log-rank检验组间生存曲线差异,Cox比例风险模型用于评估各影响因素对生存率的影响。所有统计检验均为双侧检验,P<0.05表示差异有统计学意义。
2 结 果
2.1 老年乳腺癌的临床、病理特征
内科合并症指伴有高血压、高血脂、糖尿病、风湿性心脏病、冠心病、主动脉粥样硬化等病变。年龄越大,伴有内科合并症的概率越高(P=0.009),ER/PR的表达概率越高(P=0.045),接受辅助化疗的概率越低(P=0.008)。组织学分级、肿瘤的大小、淋巴结转移的状况、HER2的表达、手术方式、放疗、内分泌治疗与年龄无明显关系(P>0.05)。(见表1)。
2.2 预后特征
所有患者的中位随访期为85个月,随访期间复发、转移共有13例;10例患者死亡,其中7例死于乳腺癌远处转移,3例死于心脑血管病、糖尿病并发症。无病生存率为82.2%;总生存率86.3%。其中≥70岁、65~69岁无病生存率分别为83.9%、81.0%(P=0.879)(见图1);总生存率分别为90.3%、83.3%(P=0.600)(见图2)。
2.3 老年乳腺癌临床、病理特征与预后关系单因素分析
单因素分析发现老年乳腺癌的无病生存与肿瘤大小(P=0.020)、淋巴结转移(P=0.010)相关,总生存与HER2状态(P=0.001)相关。而无病生存、总生存与年龄、伴内科合并症、组织学分级、ER/PR状态、手术方式、辅助化疗、放疗、内分泌治疗等无明显相关(见表2)。
表1 老年乳腺癌的临床、病理特征[n(%)]
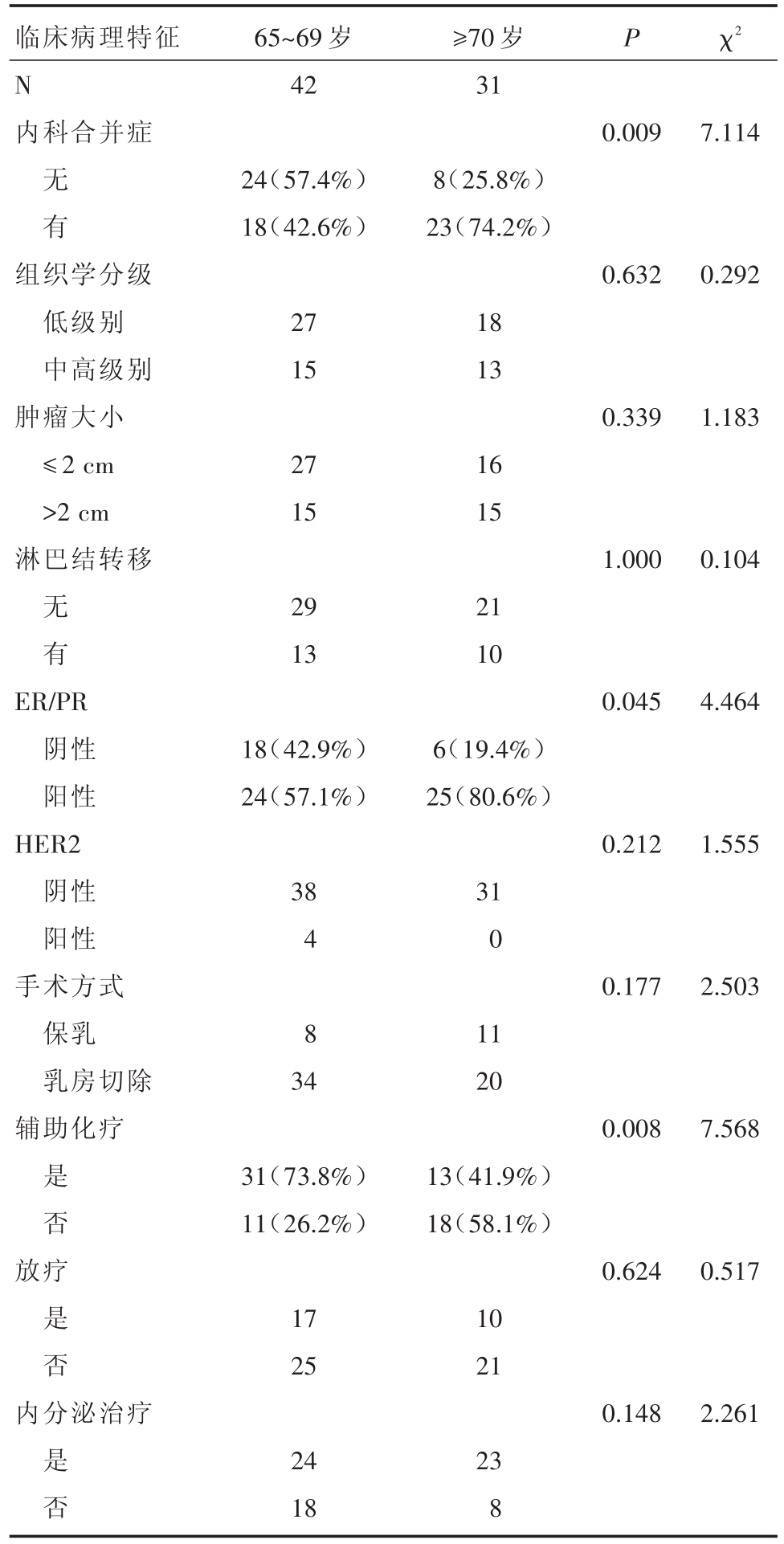
临床病理特征N内科合并症65~69岁42≥70岁31 P χ2 0.0097.114无 有24(57.4%)18(42.6%)8(25.8%)23(74.2%)组织学分级低级别中高级别肿瘤大小≤2 cm>2 cm淋巴结转移0.6320.292 27 15 18 13 0.3391.183 27 15 16 15 1.0000.104无 有29 13 21 10 ER/PR阴性阳性HER2阴性阳性手术方式保乳乳房切除辅助化疗0.0454.464 18(42.9%)24(57.1%)38 4 8 34 6(19.4%)25(80.6%)0.2121.555 31 0 0.1772.503 11 20 0.0087.568是 否31(73.8%)11(26.2%)13(41.9%)18(58.1%)放疗0.6240.517是 否17 25 10 21内分泌治疗0.1482.261是 否24 18 23 8
表2 老年乳腺癌临床、病理特征与预后关系单因素分析(n)
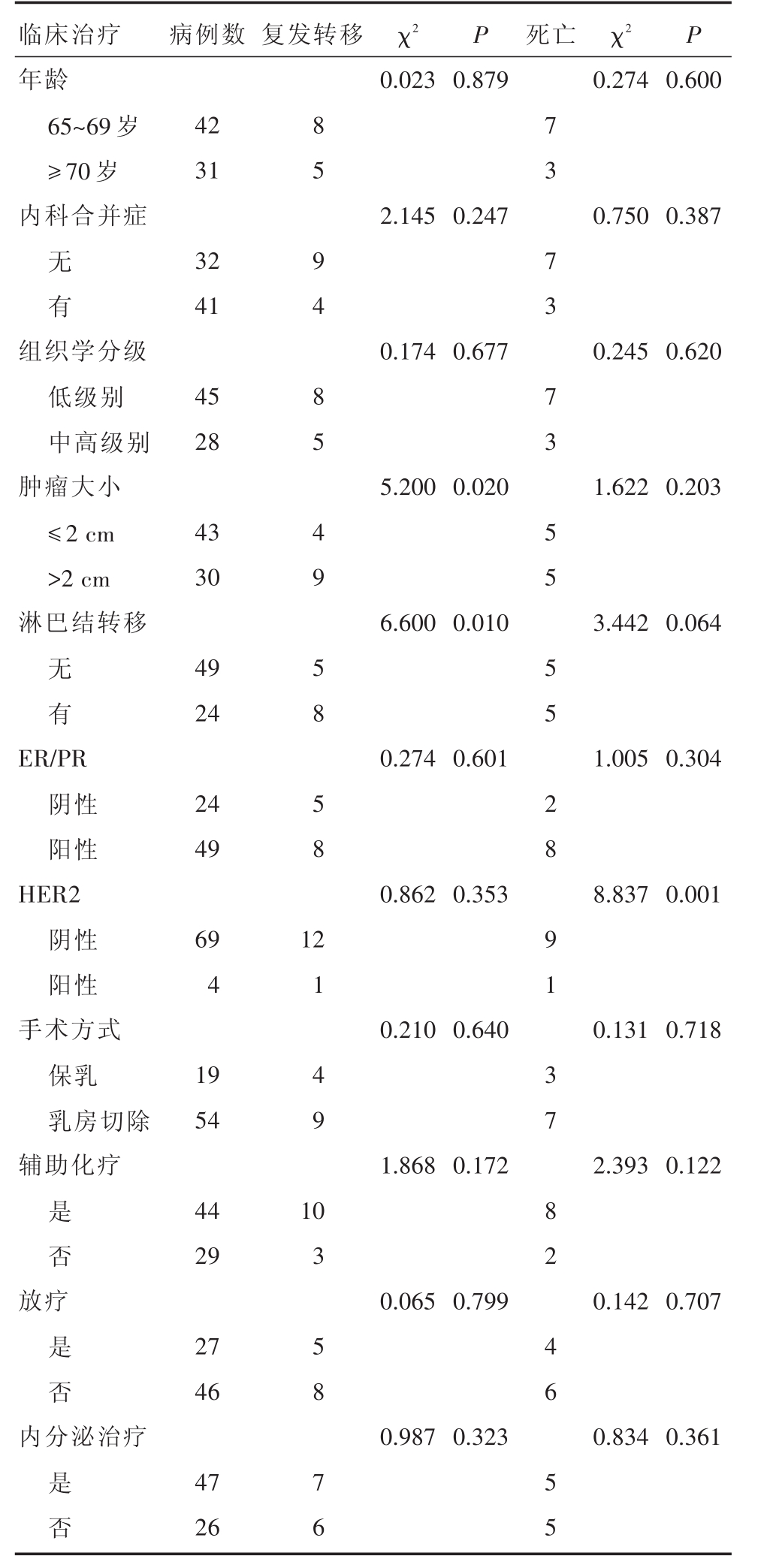
临床治疗年龄65~69岁≥70岁内科合并症病例数 复发转移 χ2P 死亡 χ2P 0.023 0.8790.274 0.600 42 31 2.145 0.2470.750 0.387无 有32 41组织学分级低级别中高级别肿瘤大小≤2 cm>2 cm淋巴结转移0.174 0.6770.245 0.620 45 28 5.200 0.0201.622 0.203 43 30 6.600 0.0103.442 0.064无 有49 24 ER/PR阴性阳性HER2阴性阳性手术方式保乳乳房切除辅助化疗0.274 0.6011.005 0.304 24 49 0.862 0.3538.837 0.001 69 4 8 5 9 4 8 5 4 9 5 8 5 8 1 0.210 0.6400.131 0.718 19 54 1.868 0.1722.393 0.122是 否44 29 2 1 4 9 1放疗0.065 0.7990.142 0.707是 否27 46内分泌治疗0.987 0.3230.834 0.361是 否47 26 0 3 5 8 7 6 7 3 7 3 7 3 5 5 5 5 2 8 9 1 3 7 8 2 4 6 5 5
2.4 老年乳腺癌临床、病理特征与预后关系多因素分析
多因素分析发现老年乳腺癌的预后与年龄、合并症、肿瘤大小、淋巴结状态、ER/PR、HER2、手术方式、辅助化疗、放疗、内分泌治疗无明显关系(见表3)。
表3 老年乳腺癌临床、病理特征与预后关系多因素分析
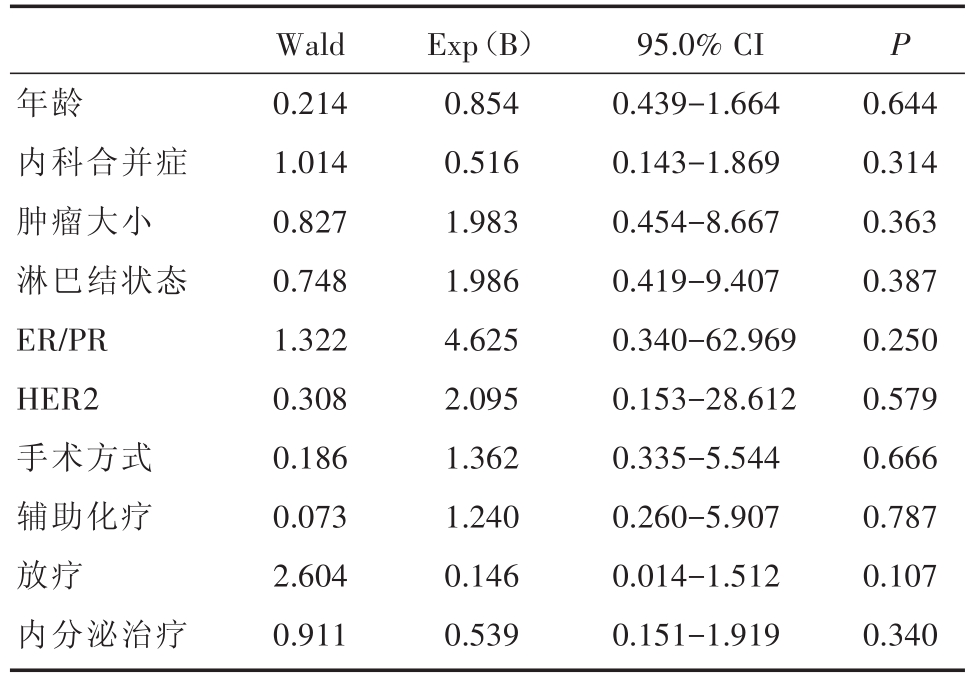
年龄内科合并症肿瘤大小淋巴结状态ER/PR HER2手术方式辅助化疗放疗内分泌治疗Wald 0.214 1.014 0.827 0.748 1.322 0.308 0.186 0.073 2.604 0.911 Exp(B)0.854 0.516 1.983 1.986 4.625 2.095 1.362 1.240 0.146 0.539 95.0%CI 0.439-1.664 0.143-1.869 0.454-8.667 0.419-9.407 0.340-62.969 0.153-28.612 0.335-5.544 0.260-5.907 0.014-1.512 0.151-1.919 P 0.644 0.314 0.363 0.387 0.250 0.579 0.666 0.787 0.107 0.340
3 讨论
本研究发现老年乳腺癌的生物学特性相对较好,预后也相对较好,中位随访期为85个月,无病生存率达82.2%,总生存率达86.3%。本研究中老年乳腺癌的生物学特性主要表现为大部分肿瘤≤2 cm、组织学分级多为低级别、分期较早(59%为Ⅰ期乳腺癌)、腋窝淋巴结阴性。这可能与我院开展早期乳腺癌筛查和新的诊疗技术如乳管镜、病灶经皮活检(乳腺X线摄片下钙化灶钢丝定位活检、亚临床病灶经皮真空辅助旋切微创手术活检等)、乳腺专用磁共振等有关[4-6]。在单因素分析中发现肿瘤大小和淋巴结转移和乳腺癌预后相关,可见早期乳腺癌的检出可影响老年乳腺癌的预后。本研究发现老年乳腺癌主要是ER/PR阳性乳腺癌为主,HER2阳性率极低,特别是≥70岁的患者,ER/PR阳性率超过80%,国外文献也提示老年乳腺癌主要以ER/PR阳性乳腺癌为主[7],并且进一步分析发现年龄并不是乳腺癌预后的独立因素,本研究也证实了年龄并不是预测老年乳腺癌的预后独立因素。
本研究中超过50%患者伴有内科合并症,如高血压、高血脂、糖尿病、冠心病、主动脉粥样硬化等病变,特别是≥70岁的患者,伴有内科合并病的患者高达74%。国外学者Siegelmann-Danieli等也研究显示,在992例70岁以上老年乳腺癌患者中,伴有内科合并症的患者占87%,其中有3种以上合并症的患者占44%[8]。虽然本研究中有3例患者死于内科合并症,但伴有内科合并症并未对乳腺癌预后有影响。同时伴有内科合并症可能会影响老年乳腺癌的外科、化疗、放疗等治疗。研究表明随着年龄越大,不接受手术治疗的概率增加,约20%的80岁以上患者不接受手术治疗,而67~69岁患者不接受手术治疗的概率仅为6%。随着年龄增大,选择保乳手术的概率也在增加[9]。然而有研究表明老年患者通常对手术的耐受良好,并且并发症率低,术后主要并发症(大部分为伤口愈合不良)发生率约6%[10]。
CALGB 9343 trial研究表明,≥70岁患者保乳术后接受放疗10年的复发率低于不接受放疗(2%vs.10%),但对总生存没有影响[11]。本研究显示年龄越大,接受辅助化疗患者的也少,65~69岁患者接受辅助化疗的比率为73.8%,而≥70岁患者仅为41.9%,国内尚有研究提示大于80岁患者仅为17.2%[12],但本研究显示是否接受辅助化疗并不影响老年乳腺癌的预后。2005年Early Breast Cancer Trialists′Collaborative Group(EBCTCG)结果显示化疗使<50岁乳腺癌患者15年死亡率降低38%,而50~69岁的患者死亡率降低仅20%,提示随着年龄的增长,化疗获益逐渐减少[13]。并且文献显示化疗毒副作用及化疗相关死亡率随着年龄而增加,50岁以下、50~64岁、64岁以上AML的发生率和化疗相关死亡率分别为0.3%、0.7%、1.8%和0.2%、0.4%、1.5%[14]。因老年乳腺癌患者多伴有内科合并症,发生化疗的相关死亡风险增加,因此选择辅助化疗时应权衡利弊,目前21基因检测可能对老年乳腺癌权衡是否接受化疗很好的指导意义[15]。虽然本研究中HER2阳性率不高,而单因素分析中发现其与老年乳腺癌的总生存率相关,一些研究显示HER2阳性乳腺癌组织中存在胰岛素样生长因子-Ⅱ受体(insulin-like growth factor-Ⅱreceptor,IGF-II R),预示着预后更差[16]。但研究中HER2阳性的患者仅有4例,例数太少,结果值得商榷。目前对于HER2阳性的老年乳腺癌患者行曲妥珠单抗治疗的临床研究资料相当有限。
综上所述,老年乳腺癌患者大部分为肿瘤≤2 cm、组织学分级为低级别、腋窝淋巴结阴性、激素受体阳性和HER2阴性,具有肿瘤生物学特性较好等特点,在单因素分析中发现肿瘤大小、HER2和淋巴结转移与乳腺癌预后相关。老年乳腺癌患者多伴有内科合并症、健康状况较差,应根据患者意愿、全身情况和肿瘤特性等决定了其治疗更应遵循个体化原则。以外科手术治疗特别是保乳术在老年早期乳腺癌的综合治疗中仍是重要的治疗手段,全面综合评估患者的耐受性和获益程度选择放化疗、放疗及内分泌治疗等治疗。
参考文献
[1] Richardson LC,Henley SJ,Miller JW,et al.Patterns and trends in age-specific black-white differences in breast cancer incidenceand mortality-United States,1999-2014[J].MMWR Morb Mortal Wkly Rep,2016,65(40):1093-1098.
[2] Fan L,Strasser-Weippl K,Li JJ,et al.Breast cancer in China[J].Lancet Oncol,2014,15(7):e279-289.
[3] 王永南,李文萍,于海云,万舰.老年乳腺癌术后辅助化疗对预后的影响[J].岭南现代临床外科,2017,17(2):198-201.
[4] 朱彩霞,王颀,邓群娣,等.纤维乳管镜检查分级在乳头血性溢液疾病诊断中的应用价值[J].中华乳腺病杂志(电子版),2011,5(2):171-179.
[5] 王永南,王颀,张安秦,等.真空辅助旋切微创术对超声检查良肿块的诊治价值[J].中华乳腺病杂志(电子版),2010,4(4):403-409.
[6] 张安秦,王颀,朱彩霞,等.Mammotome手术诊治乳腺不可触及病灶的研究[J].中国微创外科杂志,2009,9(1):24-26.
[7] Jenkins EO,Deal AM,Anders CK,et al.Age-specific changes in intrinsic breast cancer subtypes:a focus on older women[J].Oncologist,2014,19(10):1076-1083.
[8] Gennari R,Curigliano G,Rotmensz N,et al.Breast carci-noma in elderly women:features of disease presentation,choice of local and systemic treatments compared with younger postmenopausal patients[J].Cancer,2004,101(6):1302-1310.
[9] Schonberg MA,Marcantonio ER,Li D,Silliman RA,et al.Marcantonio,breast cancer among the oldest old:tumor characteristics,treatment choices,and survival[J].J Clin Oncol,2010,28(12):2038-2045.
[10]Chatzidaki P,Mellos C,Briese V,et al.Perioperative complications of breast cancer surgery in elderly women(≥80 years)[J].Ann Surg Oncol,2011,18(4):923-931.
[11]Hughes KS,Schnaper LA,Bellon JR,et al.Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer:long-term follow-up of CALGB 9343[J].JClin Oncol,2013,31(19):2382-2387.
[12]吕庆,金琳芳,孟东.58例年龄大于80岁乳腺癌的临床病理分析及诊治体会[J].中华内分泌外科杂志,2015,9(5):385-389.
[13] Early Breast Cancer Trialists′Collaborative Group(EBCTCG).Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival:an overview of the randomised trials[J].Lancet,2005,365(9472):1687-1717.
[14]Muss HB,Berry DA,Cirrincione C,et al.Toxicity of older and younger patients treated with adjuvant chemotherapy for node-positive breast cancer:the cancer and leukemia group B experience[J].JClin Oncol,2007,25(24):3699-3704.
[15]鲁凯,刘燕文,李惠,等.21基因检测对乳腺癌预测和预后的研究[J].中华内分泌外科杂志,2015,9(5):376-379.
[16]陆翔,陈彩萍,邬万新,等.HER2阳性乳腺癌组织胰岛素样生长因子-Ⅱ受体的表达与预后的关系[J].中华内分泌外科杂志,2013,7(5):379-383.

