急性肿瘤溶解综合征(tumor lysis syndrome,TLS)是最常见的肿瘤急症,几乎在每一种癌症类型中都有报道,发病率差别很大[1]。TLS的发生原因是肿瘤细胞裂解和细胞死亡内物质释放导致的代谢紊乱,其主要风险与高代谢率的肿瘤有关,主要发生在具有巨大的肿瘤负荷的淋巴瘤和白血病患者,而在实体瘤或生长速度缓慢的血液系统恶性肿瘤(如多发性骨髓瘤)发生TLS的风险较低[2]。TLS主要影响电解质代谢和肾脏,可产生严重和潜在的致命后果,与其相关的最常见的电解质异常包括高钾血症、高磷血症和低钙血症;急性肾损伤(AKI)则由多种因素引起,包括尿酸结晶和磷酸钙的肾小管沉积和肾血流灌注的改变[3]。
1 流行病学资料
TLS主要发生在血液系统恶性肿瘤患者,伴有肿瘤大、快速生长和对化疗敏感,如急性淋巴细胞白血病(ALL)风险最大,超过四分之一的罹患该病的儿童治疗后可能发展成TLS[4];成人中则在急性髓系白血病和Burkitt淋巴瘤中最常见[1]。TLS的总死亡率为29%~79%,但早发现及早干预可明显降低死亡率[5,6]。
TLS常与细胞毒治疗相关,也有在放疗、地塞米松治疗、沙利度胺治疗和使用新的化疗药物(包括硼替佐米和利妥昔单抗)后发生 TLS报道[7,8]。在过去十年中,实体瘤发生TLS的病例报告越来越多,这可能与提高肿瘤的干预措施或加强了监测有关,说明TLS的风险并不局限于血液恶性肿瘤患者。最近的病例报告包括肝细胞癌[9]、肺[10]及转移性前列腺癌患者中发生TLS[11],以及一例抗生素用后的内脏利什曼病病的TLS样高尿酸血症状态[13]。而根据 Baeksgaard 等[12]2003 年报告,所有文献中仅检索到45例实体瘤患者发生TLS,大多数为转移性肿瘤。总之,任何细胞的快速溶解都可能会导致一些物质向细胞外空间的大量转移并引起这种病理综合征。
2 临床特征和诊断共识
目前还没有通用的TLS定义,临床常常采用Cairo和Bishop的实验室和临床特点作为诊断指标[15]。生化诊断包括两个或多个以下标准:在化疗开始前或开始后7天内同时发生高尿酸血症、高钾血症、高磷血症、低钙血症;实验室检查异常合并AKI(血清肌酐升高超过基线水平的1.5倍)、癫痫发作、心律失常或死亡时,TLS诊断成立。但这个标准对自发性TLS的诊断没有帮助(表1)。TLS在肿瘤细胞破坏引起的核酸迅速降解,在化疗给药期间或细胞毒治疗后7天内发生,导致电解质紊乱,所有这些异常都会导致致命的后果。两个相关的并发症是危及生命的心律失常(由于电解质失衡)和AKI(由于高尿酸血症或高尿酸血症)。
患者发病时的主要表现包括疲劳、恶心和呕吐、脱水、癫痫发作、心脏失常等。
表1 肿瘤溶解综合征临床和实验室的Cairo-Bishop标准[15]

实验室标准(在化疗前3天或化疗后7天内达到以下两个或两个以上标准)临床标准(TLS实验室标准加上以下一种或多种)尿酸:>476μmol/L或基线增加25%钾:>6 mEq/L或基线增加25%磷:儿童:≥2.1 mmol/L,成人:1.45 mmol/L,或基线增加5%钙:≤1.75 mmol/L或基线下降到25%肌酐>年龄调整参考范围上限的1.5倍心律失常或猝死癫痫
3 危险因素
目前,TLS危险分层主要围绕恶性肿瘤,但一些因素明显增加了TLS的可能性,表2、表3列出了TLS的危险因素并进行说明。在相关文献报道中TLS发生在有肾脏疾病的患者中更为常见。一项对近1200名儿童非霍奇金淋巴瘤患者的研究显示,在63名TLS患者中,43名患者入院时有肾功能不全的迹象,其肾功能不全的病因尚不清楚[16];另一组数据中,在新诊断为急性髓系白血病的成人患者中,平均肌酐浓度大于124μmol/L对TLS的发展具有很强的预测作用(OR=10.7,95%CI:4.5-25.1)[17]。虽然TLS预防性措施不是实体瘤治疗过程中的关注标准,但任何实体瘤患者伴有急性肾损伤及较大肿瘤负荷特别是在高尿酸血症、高钾血症和高磷酸盐血症中,应考虑到TLS。
表2 肿瘤溶解综合征发病率[14]

肿瘤高风险急性淋巴细胞白血病白细胞计数>75×109/L的急性髓系白血病急性B淋巴细胞白血病Burkitt′s淋巴瘤中风险急性髓系白血病,白细胞计数 25×109~50×109/L弥漫性大B细胞淋巴瘤低风险白细胞计数<25×109/L的急性髓系白血病慢性淋巴细胞白血病慢性粒细胞白血病实体瘤发病率/%5.2~23 18 26.4 14.9 6 6 1 0.33病例报告病例报告
表3 肿瘤溶解综合征的危险因素[1]
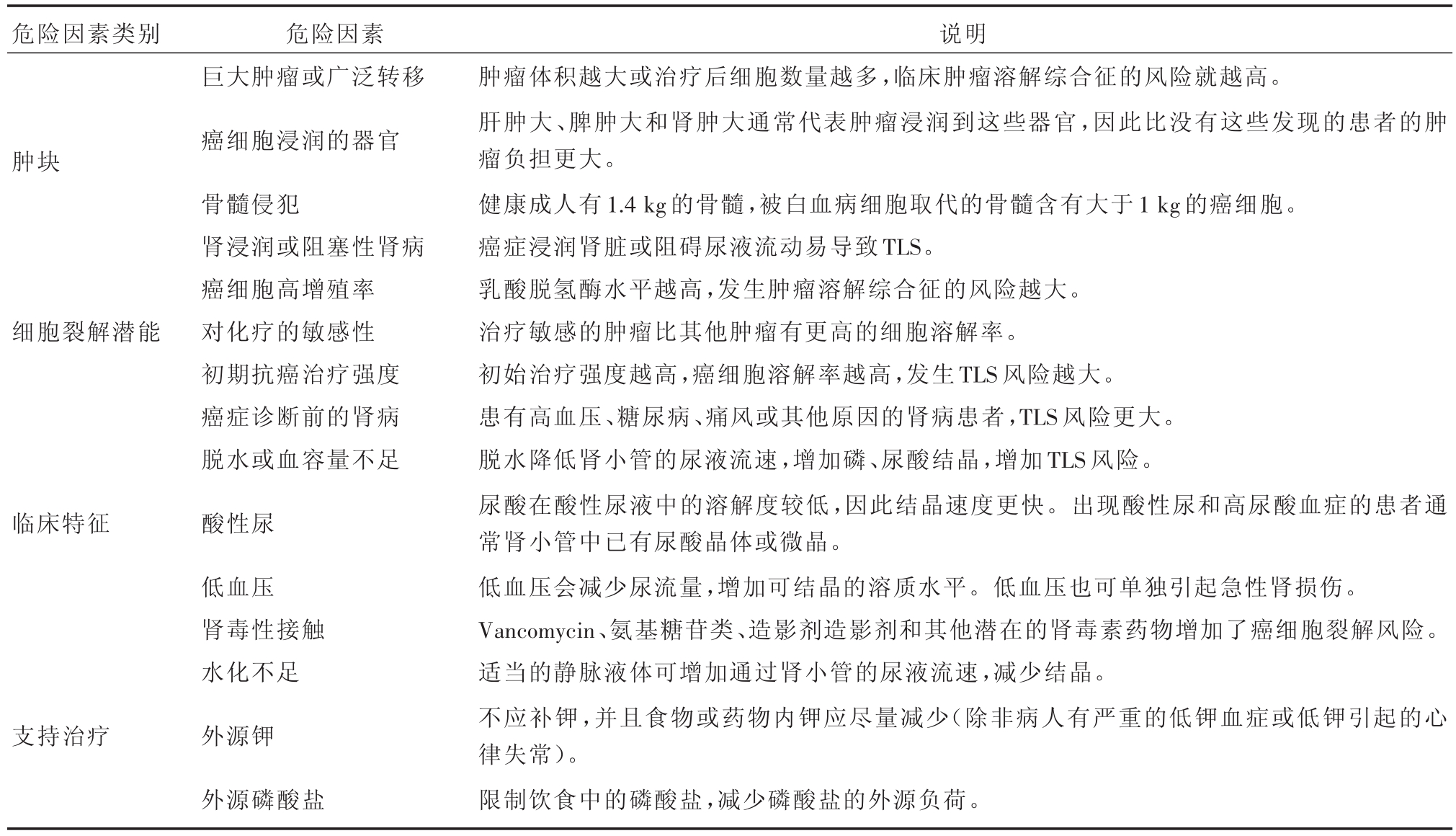
危险因素类别肿块细胞裂解潜能临床特征支持治疗危险因素巨大肿瘤或广泛转移癌细胞浸润的器官骨髓侵犯肾浸润或阻塞性肾病癌细胞高增殖率对化疗的敏感性初期抗癌治疗强度癌症诊断前的肾病脱水或血容量不足酸性尿低血压肾毒性接触水化不足外源钾外源磷酸盐说明肿瘤体积越大或治疗后细胞数量越多,临床肿瘤溶解综合征的风险就越高。肝肿大、脾肿大和肾肿大通常代表肿瘤浸润到这些器官,因此比没有这些发现的患者的肿瘤负担更大。健康成人有1.4 kg的骨髓,被白血病细胞取代的骨髓含有大于1 kg的癌细胞。癌症浸润肾脏或阻碍尿液流动易导致TLS。乳酸脱氢酶水平越高,发生肿瘤溶解综合征的风险越大。治疗敏感的肿瘤比其他肿瘤有更高的细胞溶解率。初始治疗强度越高,癌细胞溶解率越高,发生TLS风险越大。患有高血压、糖尿病、痛风或其他原因的肾病患者,TLS风险更大。脱水降低肾小管的尿液流速,增加磷、尿酸结晶,增加TLS风险。尿酸在酸性尿液中的溶解度较低,因此结晶速度更快。出现酸性尿和高尿酸血症的患者通常肾小管中已有尿酸晶体或微晶。低血压会减少尿流量,增加可结晶的溶质水平。低血压也可单独引起急性肾损伤。Vancomycin、氨基糖苷类、造影剂造影剂和其他潜在的肾毒素药物增加了癌细胞裂解风险。适当的静脉液体可增加通过肾小管的尿液流速,减少结晶。不应补钾,并且食物或药物内钾应尽量减少(除非病人有严重的低钾血症或低钾引起的心律失常)。限制饮食中的磷酸盐,减少磷酸盐的外源负荷。
4 病理生理学
TLS的代谢紊乱包括高钾血症、高磷血症、低钙血症和高尿酸血症(表4):①高钾血症是急性TLS最严重的表现,是最初危及生命的主要因素[18],在细胞毒性治疗开始后6~72小时内出现,而且急性肾损伤后进一步加重这一过程[19]。高钾血症可由两种不同的机制引起。首先,在细胞膜上存在钠-钾三磷酸腺苷酶(Na+-K+ATPase)调节的钾梯度,化疗或放疗时,细胞代谢增加,三磷酸腺苷(ATP)以更高的速率消耗,因此几乎没有剩余的ATPase来维持钾的梯度,导致K+在肿瘤细胞裂解之前离开细胞而形成高钾血症[20]。高钾血症的另外一种机制是在肿瘤细胞裂解后释放细胞内的K+。②低钙血症是继发于细胞裂解释放的磷酸盐,血液系统恶性肿瘤细胞内磷酸盐含量是正常淋巴细胞的4倍[21],低钙血症不仅可导致手足搐和癫痫发作,还可导致致命性心律失常。化疗可阻止磷的再利用[22],在血磷水平超过肾脏排出磷酸盐的能力之前,血液中磷含量的显著升高是看不到的,其通常在开始治疗24~48小时后发生。过量的磷酸盐与游离钙结合导致低钙血症,急性磷酸盐负荷可导致磷酸钙结晶尿和梗阻性肾病、肾小管内钙质沉着症。③核酸在细胞裂解后释放到血液中,并被黄嘌呤氧化酶转化为尿酸,大量尿酸生成导致肾小管尿酸结晶沉淀[23]。高尿酸血症通常在化疗开始后48~72小时发生[18]。
5 TLS急诊处理
5.1 水化作用和电解质紊乱
一旦TLS确认,最初的干预措施包括积极的静脉输液和纠正电解质异常。建议等渗液体复苏,目标为成人和儿童每天至少2000~3000 mL/m2,(对于小于10公斤的儿童每天使用200 mL/kg)[25,26]。高钾血症应该是治疗的重点,通常可用肠内聚苯乙烯钠治疗,但由于离子交换树脂起效缓慢,有症状的病人需要更快速的治疗,如应用胰岛素和葡萄糖或碳酸氢钠使钾在细胞内移动,葡萄糖酸钙使心肌细胞膜稳定[18,27]。对于严重或难治性TLS,碳酸氢钠应谨慎使用,以避免意外的高血容量、代谢性碱中毒或钙沉淀。磷酸盐胶粘剂如氢氧化铝(300~600 mg,口服)可用于治疗磷酸盐水平超过6 mg/dL的稳定患者中的过量磷[25]。症状性低钙血症(癫痫发作、手足搐动或心律失常)应用静脉注射1 g葡萄糖酸钙,剂量可按症状管理所需重复(表5)对于TLS,额外的钙可能引起磷酸钙沉淀和急性梗阻性肾病,强调无症状性低钙血症不需处理。
表4 急性肿瘤溶解综合征的代谢异常[24]

代谢异常 基线值和变化 临床提示高钾血症 ≥6.0 mmol/L或增加25%肌肉痉挛、感觉异常、心律失常室颤、心脏骤停高磷血症 儿童≥2.1 mmol/L,成人≥1.45 mmol/L,增长25%恶心、呕吐、腹泻、嗜睡、癫痫、急性肾损伤低钙血症 ≦1.75 mmol/L或减少25%肌肉痉挛、手足抽搐、低血压、心律失常高尿酸血症 ≥476 mmol/L或8 mg/dl或增加25%急性肾损伤用法聚苯乙烯磺酸钠(PSSNa)1 gm/kg胰岛素0.1 U/kg,25%葡萄糖2 mL/kg碳酸氢钠1~2 mEq/kg静脉推注葡萄糖酸钙100~200 mg/kg缓慢静脉滴注补充容积静脉输液去除磷酸盐口服磷结合剂血液透析葡萄糖酸钙50~100 mg/kg缓慢静脉滴注(有症状时给药,心电监测下输液)补充容积拉布立海(Rasburicase)0.2 mg/kg/d,iv,持续5天口服或静脉注射别嘌呤醇
5.2 高尿酸血症
别嘌呤醇通过抑制黄嘌呤氧化酶阻止尿酸的形成,通常在化疗前给药,其主要缺点包括药物超敏反应、无法清除已形成的尿酸、嘌呤积聚和有潜在可能导致肾病。目前也没有证据表明它能降低升高的肌酐水平[28]。因此,别嘌呤醇不推荐作为高危患者的一线用药。
重组尿酸盐氧化酶—拉布立酶(rasburicase)是通过将尿酸分解为溶解度更高的尿囊素而起作用,无论是治疗性还是预防性,这种药物在快速使尿酸水平正常化时都是非常有效的,且患者耐受性良好,无需调整肌酐的变化,比别嘌呤醇有更大的疗效[29,30]。对于高危易发生快速裂解的肿瘤或存在肾损伤和尿酸水平升高的高危患者推荐使用一线治疗[21]。由于过氧化氢是尿酸分解尿囊素的副产物,rasburicase在葡萄糖-6-磷酸脱氢酶缺乏症患者中可引起溶血性贫血或高铁血红蛋白血症,因此在这些患者中是禁忌的[31]。Rasburicase的建议的剂量(0.2 mg/kg,静脉注射5天)(表1)是基于预测的体重,即使是患有病态肥胖的患者[30,32]。但由于该药物的费用,使用单剂量或更短疗程的替代剂量方案不断增加[30,32,33]。虽然高尿酸血症有助于 TLS诱导的肾功能不全,但没有前瞻性随机对照试验表明尿酸氧化酶降低AKI的患病率或死亡率[34]。
非布司他(febuxostat)是非嘌呤黄嘌呤氧化酶抑制剂,在降低血清尿酸水平方面优于别嘌呤醇。它的优点是不需要对轻度或中度肾损害患者进行剂量调整[35]。针对中高TLS风险的成人(诱导化疗前2天开始,120 mg/d,持续7~9天)和儿童(诱导化疗前和化疗期间,10 mg/d,持续7天)血液恶性肿瘤患者的研究表明,非布司他坦作为TLS预防的一种手段,在控制血清尿酸水平方面明显比别嘌呤醇更有效[36]。
5.3 肾脏替代疗法
急性TLS的中高尿酸血症、高钾血症和高磷酸盐血症、AKI以及不接受医疗治疗的患者,在某些情况下如发生心力衰竭,采取控制性液体复苏,需要实施肾脏替代疗法。鉴于TLS来源于钾、磷和尿酸的连续释放,应首选肾替代疗法的连续模式,以降低反弹性高钾血症和高磷酸盐血症的风险。此外,为防止这种反弹效应,在危及生命的高钾血症患者中,建议早期进行。对于AKI患者的高磷血症,优先选择连续置换治疗。但连续性肾脏替代是否比间歇性治疗更有效尚不清楚[18]。
6 总结
TLS是一种肿瘤急症,其特征是高尿酸血症、肾功能损害和电解质紊乱严重时可危及生命。TLS预后取决于疾病严重程度和电解质失衡的改善情况。急诊医生应该认识TLS及其风险程度,疑似病例应快速完善TLS相关检查,及早治疗。必要时请专科会诊共同治疗。
参考文献
[1] Howard SC,Jones DP,Pui CH.The tumor lysis syndrome[J].N Engl JMed,2011,364(19):1844-1854.
[2] Khan UA,Shanholtz CB,McCurdy MT.Oncologic Mechanical Emergencies[J].Hematol Oncol Clin North Am,2017,31(6):927-940.
[3] Criscuolo M,Fianchi L,Dragonetti G,Pagano L.Tumor lysis syndrome:review of pathogenesis,risk factors and management of a medical emergency[J].Expert Rev Hematol,2016,9(2):197-208.
[4] Wössmann W,Schrappe M,Meyer U,et al.Incidence of tumor lysis syndrome in children with advanced stage Burkitt′s lymphoma/leukemia before and after introduction of prophylactic use of urate oxidase[J].Ann Hematol,2003,82(3):160-165.
[5] Howard SC,Jones DP,Pui CH.The tumor lysis syndrome[J].N Engl JMed,2011,364(19):1844-1854.
[6] Belay Y,Yirdaw K,Enawgaw B.Tumor lysis syndrome in patients with hematological malignancies[J].J Oncol,2017,2017:9684909.
[7] Noh GY,Choe DH,Kim CH,Lee JC.Fatal tumor lysis syndrome during radiotherapy for nonsmall-cell lung cancer[J].J Clin Oncol,2008,26(36):6005-6006.
[8] Lipstein M,O′Connor O,Montanari F,et al.Bortezomibinduced tumor lysis syndrome in a patient with HIV-negative plasmablastic lymphoma[J].Clin Lymphoma Myeloma,2010,10(5):E43-E46.
[9] Chao CT,Chiang CK.Rasburicase for huge hepatocellular carcinoma with tumor lysis syndrome:case report[J].Med Princ Pract,2012,21(5):498-500.
[10]Stuart S,Auten J.A rare seizure:Tumor lysis syndrome after radiation therapy of a solid tumor[J].Am J Emerg Med,2017,35(6):941.e3-941.e4.
[11]Kaplan MA,Kucukoner M,Alpagat G,Isikdogan A.Tumor lysis syndrome during radiotherapy for prostate cancer with bone and bone marrow metastases without visceral metastasis[J].Ann Saudi Med,2012,32(3):306-308.
[12]Baeksgaard L,Sorensen JB.Acute tumor lysis syndrome in solid tumors-a case report and review of the literature[J].Cancer Chemother Pharmacol,2003,51(3):187-192.
[13]Liberopoulos EN,Kei AA,Elisaf MS.Lysis syndrome during therapy of visceral leishmaniasis[J].Infection,2012,40(2):121-123.
[14] Wilson FP,Berns JS.Tumor lysis syndrome:new challenges and recent advances[J].Adv Chronic Kidney Dis,2014,21(1):18-26.
[15]Cairo MS,Bishop M.Tumour lysis syndrome:new therapeutic strategies and classification[J].Br JHaematol,2004,127(1):3-11.
[16]Seidemann K,Meyer U,Jansen P,et al.Impaired renal function and tumor lysis syndrome in pediatric patients with non-Hodgkin′s lymphoma and B-ALL.Observations from the BFM-trials[J].Klin Padiatr,1998,210(4):279-284.
[17]Montesinos P,Lorenzo I,Martin G,et al.Tumor lysis syndrome in patients with acute myeloid leukemia:identification of risk factors and development of a predictive model[J].Haematologia,2008,93(1):67-74.
[18] Flombaum C.Metabolic emergencies in the cancer patient[J].Semin Oncol,2000,27(3):322-334.
[19]Davidson MB,Thakkar S,Hix JK,et al.Pathophysiology,clinical consequences,and treatment of tumor lysis syndrome[J].Am JMed,2004,116(8):546-554.
[20] Chasty R,Liu-Yin J.Acute tumour lysis syndrome[J].Br J Hosp Med,1993,49(7):488-492.
[21]Coiffier B,Altman A,Pui CH,et al.Guidelines for the management of pediatric and adult tumor lysis syndrome:an evidencebased review[J].JClin Oncol,2008,26(16):2767-2778.
[22] Koduri PR.Hyperphosphatemia and tumor lysis syndrome[J].Ann Hematol,2005,84(10):696.
[23]Lameire NH,Flombaum CD,Moreau D,Ronco C.Acute renal failure in cancer patients[J].Ann Med,2005,37(1):13-25.
[24] McCurdy MT,Shanholtz CB.Oncologic emergencies[J].Crit Care Med,2012,40(7):2212-2222.
[25]Will A,Tholouli E.The clinical management of tumour lysis syndrome in haematological malignancies[J].Br J Haematol,2011,154(1):3-13.
[26]El-Husseini A,Sabucedo A,Lamarche J,et al.Acute kidney injury associated with tumor lysis syndrome:a paradigm shift[J].Am Emerg Med,2012,30(2):390.e3-6.
[27]Hsu HH,Huang CC.Acute spontaneous tumor lysis in anaplastic large T-cell lymphoma presenting with hyperuricemic acute renal failure[J].Int JHematol,2004,79(1):48-51.
[28]Smalley RV,Guaspari A,Haase-Statz S,et al.Allopurinol:Intravenous use for prevention and treatment of hyperuricemia[J].JClin Oncol,2000,18(8):1758-1763
[29]Jeha S,Kantarjian H,Irwin D,et al.Efficacy and safety of rasburicase,a recombinant urate oxidase(Elitek),in the management of malignancy-associated hyperuricemia in pediatric and adult patients:Final results of a multicenter compassionate use trial[J].Leukemia,2005,19(1):34-38.
[30]Patel KS,Lau JE,Zembillas AS,Gallagher EM.Single 4.5 mg fixed-dose of rasburicase for hyperuricemia associated with tumor lysis syndrome[J].J Oncol Pharm Pract,2017,23(5):333-337.
[31]Khan M,Paul S,Farooq S,et al.Rasburicase-Induced Methemoglobinemia in a Patient with Glucose-6-Phosphate Dehydrogenase Deficiency[J].Curr Drug Saf,2017,12(1):13-18.
[32]Arnold TM,Reuter JP,Delman BS,et al.Use of single-dose rasburicase in an obese female[J].Ann Pharmacother,2004,38(9):1428-1431.
[33]Herrington JD,Dinh BC.Fixed,low-dose rasburicase for the treatment or prevention of hyperuricemia in adult oncology patients[J].JOncol Pharm Pract,2015,21(2):111-117
[34]Galardy PJ,Hochberg J,Perkins SL,et al.Rasburicase in the prevention of laboratory/clinical tumour lysis syndrome in children with advanced mature B-NHL:a Children′s Oncology Group Report[J].Br JHaematol,2013,163(3):365-372.
[35]Takano Y,Hase-Aoki K,Horiuchi H,et al.Selectivity of febuxostat,a novel nonpurine inhibitor of xanthine oxidase/xanthine dehydrogenase[J].Life Sci,2005,76(16):1835-1847.
[36]Kishimoto K,Kobayashi R,Hori D,et al.Febuxostat as a Prophylaxis for Tumor Lysis Syndrome in Children with Hematological Malignancies[J].Anticancer Res,2017,37(10):5845-5849.

