急性胆管炎是一种潜在的全身感染性疾病,有时可迅速发展至感染性休克、甚至发生多器官功能衰竭而致死[1]。尽管目前国内外指南[2,3]以解除胆道梗阻作为急性胆管炎的治疗金标准,但抗菌药物的治疗仍然占有极其重要的地位。有研究[3]认为经验性抗生素的使用与否是急性胆管炎死亡的独立危险因素。近期急性胆管炎患者胆汁培养的致病菌及其药敏情况是选择抗生素时最为重要的参考因素。因此本研究回顾性分析2015年1月~2018年1月湛江地区我院收治符合病例研究纳入标准共314例急性胆管炎患者的临床病例资料,对其术中胆汁培养的病原菌分布及耐药性进行分析,以期为急性胆管炎患者提供更为合理的经验性抗生素的治疗。
1 资料与方法
1.1 临床资料与病例纳入标准
1.1.1 病例纳入标准 ①年龄18至90岁患者;②入院时诊断符合2013版东京指南关于急性胆管炎诊断标准:炎症表现(A)、淤胆情况(B)、影像学检查(C)三个方面:A炎症反应:A-1发烧(T>38℃)和(或)寒战,A-2实验室数据:炎症反应(WBC<4×109/L,or>10×109/L;CRP≥1 mg/dL);B淤胆情况:B-1:黄疸(总胆红素≥2 mg/dL),B-2,实验数据:肝功能异常检查(血清ALP、r-GTP、AST和ALT大于正常值上限的1.5倍);C影像学表现:C-1:胆道扩张,C-2影像学病因(狭窄、结石、支架等)明确诊断:A+B+C(A、B、C中只需一项);③具有完整胆汁收集手术记录;④收集2015年1月~2018年1月湛江地区我院收治符合病例研究纳入标准的病例。
1.1.2 病例排除标准 ①病例资料不完整;②合并其他部位的慢性或重症感染;③合并其他免疫性疾病;④胆汁培养结果非术中留取结果;⑤特殊人群(婴幼儿、孕妇及哺乳期妇女)。
1.2 方法
1.2.1 获取胆汁的方法 行腹腔镜下胆总管切开探查取石手术时,腔镜下探查后,立即用腹腔镜穿刺针抽取胆总管5~10 mL胆汁记录其颜色及性状后注入专用培养皿送检验科及细菌室行胆汁培养及药敏。
1.2.2 行开腹胆总管切开探查取石手术时,入腹常规探查后,立即用10 mL注射器穿刺胆总管抽取5~10 mL胆汁记录其颜色及性状后注入专用培养皿送检验科及细菌室行胆汁培养及药敏。
1.2.3 胆汁培养的方法及药敏试验 检验科技术人员将收集到的胆汁于双相血培养瓶中37?C培养,待液相部分变浑浊或固相部分菌落生长时转接种于血平板与中国蓝琼脂平板上,分离所得的菌株用法国生物梅里埃公司的BACT/ALERT3D及VITEK2-compact全自动血液培养系统、细菌鉴定及药敏分析仪进行鉴定及药敏测定。
1.3 数据收集与处理
收集所有纳入病例的基本资料、检验结果、药敏结果,采用SPSS 22.0软件对数据进行统计分析,计数资料采用χ2检验,计量资料采用t检验α=0.05。
2 结果
2.1 急性胆管炎胆汁培养结果
收集符合标准的急性胆管炎病例有314例,其中有细菌生长260例,阳性率82.86%。共培养出细菌358株,革兰氏阴性菌230株,革兰氏阳性菌122株,真菌6株。其中最常见的细菌是大肠埃希菌129株(36.0%)、粪肠球菌59株(16.5%)、铜绿假单胞菌27株(7.5%)、肺炎克雷伯菌肺炎亚种24株(6.7%)以及屎肠球菌17株(4.7%)铅黄肠球菌10株。在革兰阴性菌中,前3位菌依次为大肠埃希菌、铜绿假单胞菌、克雷伯菌属,分别占36.0%、7.5%、6.7%,在革兰氏阳性菌中,前3位菌依次为粪肠球菌、屎肠球菌、鹑鸡肠球菌,分别占16.5%、4.7%、3.9%。见表1。
2.2 急性胆管炎胆汁细菌药敏结果
革兰氏阴性致病菌总体上对碳氢酶烯类(厄他培南耐药率0%,亚胺培南耐药率8.41%,美罗培南
表1 胆汁培养结果
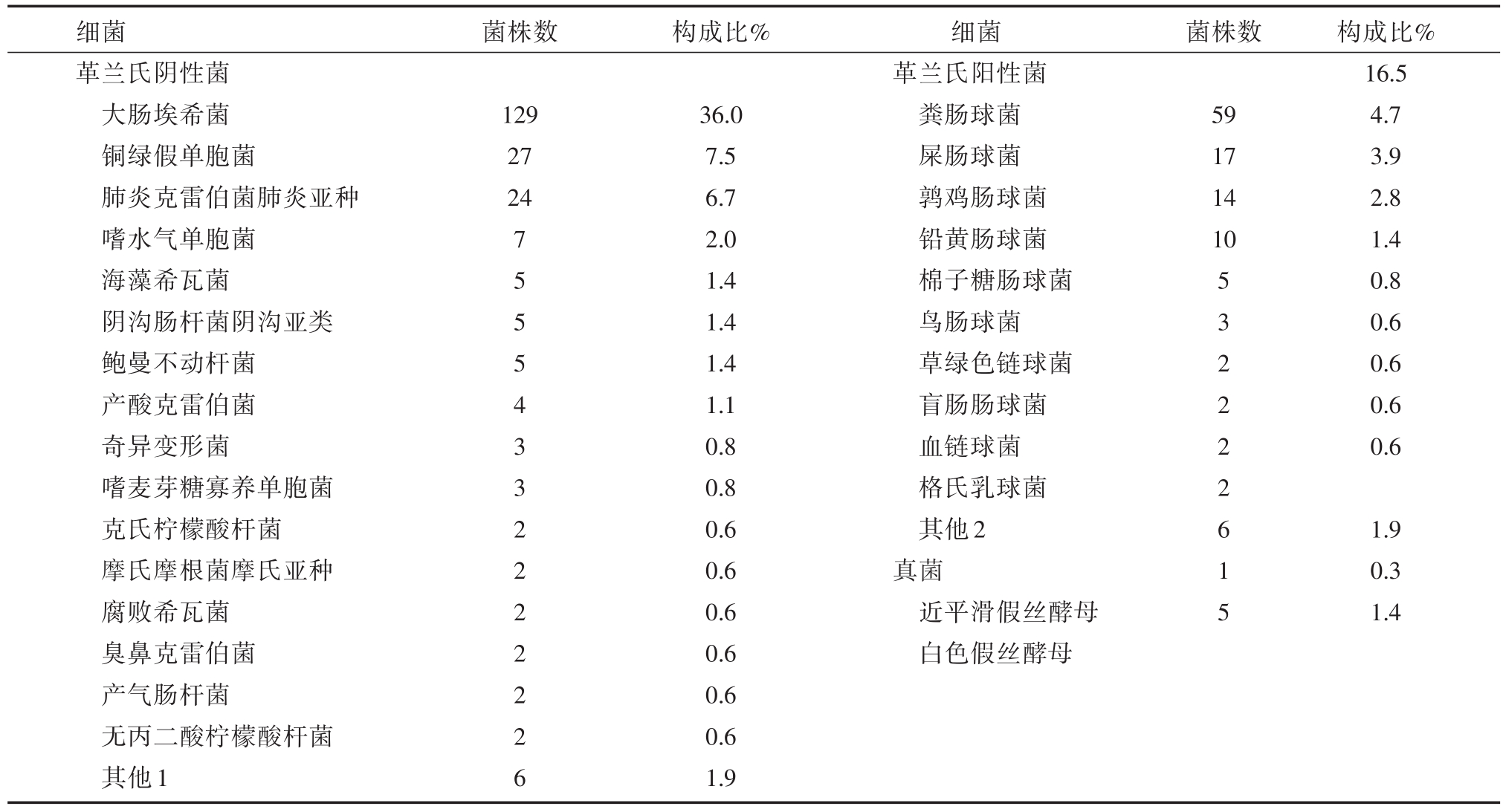
注:其他1:包括索氏志贺菌、施氏假单胞菌、杨氏柠檬酸杆菌、泛菌属、阪崎肠杆菌、恶臭假单胞菌各1例;其他2:星座链球菌亚种、溶血葡萄球菌、副血链球菌、海氏肠球菌、耐久肠球菌、无乳链球菌各1例
细菌革兰氏阴性菌大肠埃希菌铜绿假单胞菌肺炎克雷伯菌肺炎亚种嗜水气单胞菌海藻希瓦菌阴沟肠杆菌阴沟亚类鲍曼不动杆菌产酸克雷伯菌奇异变形菌嗜麦芽糖寡养单胞菌克氏柠檬酸杆菌摩氏摩根菌摩氏亚种腐败希瓦菌臭鼻克雷伯菌产气肠杆菌无丙二酸柠檬酸杆菌其他1菌株数 构成比%菌株数129 27 24 7 5 5 5 4 3 3 2 2 2 2 2 2 6 36.0 7.5 6.7 2.0 1.4 1.4 1.4 1.1 0.8 0.8 0.6 0.6 0.6 0.6 0.6 0.6 1.9细菌革兰氏阳性菌粪肠球菌屎肠球菌鹑鸡肠球菌铅黄肠球菌棉子糖肠球菌鸟肠球菌草绿色链球菌盲肠肠球菌血链球菌格氏乳球菌其他2真菌近平滑假丝酵母白色假丝酵母59 17 14 10 5 3 2 2 2 2 6 1 5构成比%16.5 4.7 3.9 2.8 1.4 0.8 0.6 0.6 0.6 0.6 1.9 0.3 1.4
耐药率22.22%)及氨基糖苷类(阿米卡星耐药率1.35%,庆大霉素耐药率20.00%、妥布霉素10.19%)相对敏感度较高。(见表2)革兰氏阳性菌对各抗生素耐药率均较好,其中对替加环素、利奈唑胺、替考拉宁、米诺环素、莫西沙星、氨苄西林、左氧氟沙星、头孢曲松耐药率低于10%。(见表3)
表2 敏感度
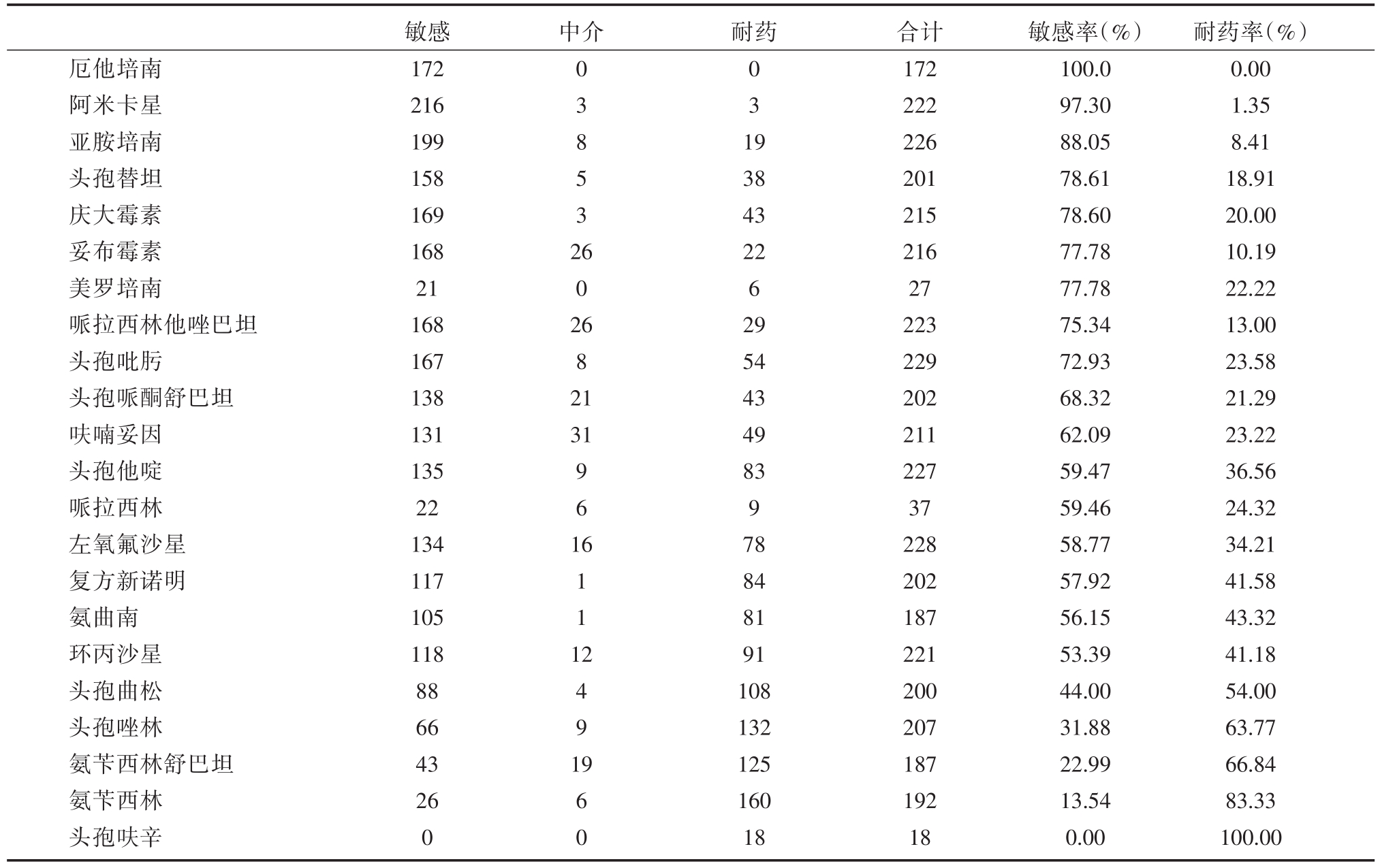
中介 耐药厄他培南阿米卡星亚胺培南头孢替坦庆大霉素妥布霉素美罗培南哌拉西林他唑巴坦头孢吡肟头孢哌酮舒巴坦呋喃妥因头孢他啶哌拉西林左氧氟沙星复方新诺明氨曲南环丙沙星头孢曲松头孢唑林氨苄西林舒巴坦氨苄西林头孢呋辛敏感172 216 199 158 169 168 21 168 167 138 131 135 22 134 117 105 118 88 66 43 26 0 0 3 8 5 3 2 0 3 1 9 6 0 2 6 8 2 1 31 9 6 1 6 1 1 1 2 4 9 1 9 6 0 38 43 22 6 29 54 43 49 83 9 78 84 81 91 108 132 125 160 18合计172 222 226 201 215 216 27 223 229 202 211 227 37 228 202 187 221 200 207 187 192 18敏感率(%)100.0 97.30 88.05 78.61 78.60 77.78 77.78 75.34 72.93 68.32 62.09 59.47 59.46 58.77 57.92 56.15 53.39 44.00 31.88 22.99 13.54 0.00耐药率(%)0.00 1.35 8.41 18.91 20.00 10.19 22.22 13.00 23.58 21.29 23.22 36.56 24.32 34.21 41.58 43.32 41.18 54.00 63.77 66.84 83.33 100.00
表3 急性胆管炎胆汁培养革兰氏阴性菌药敏结果
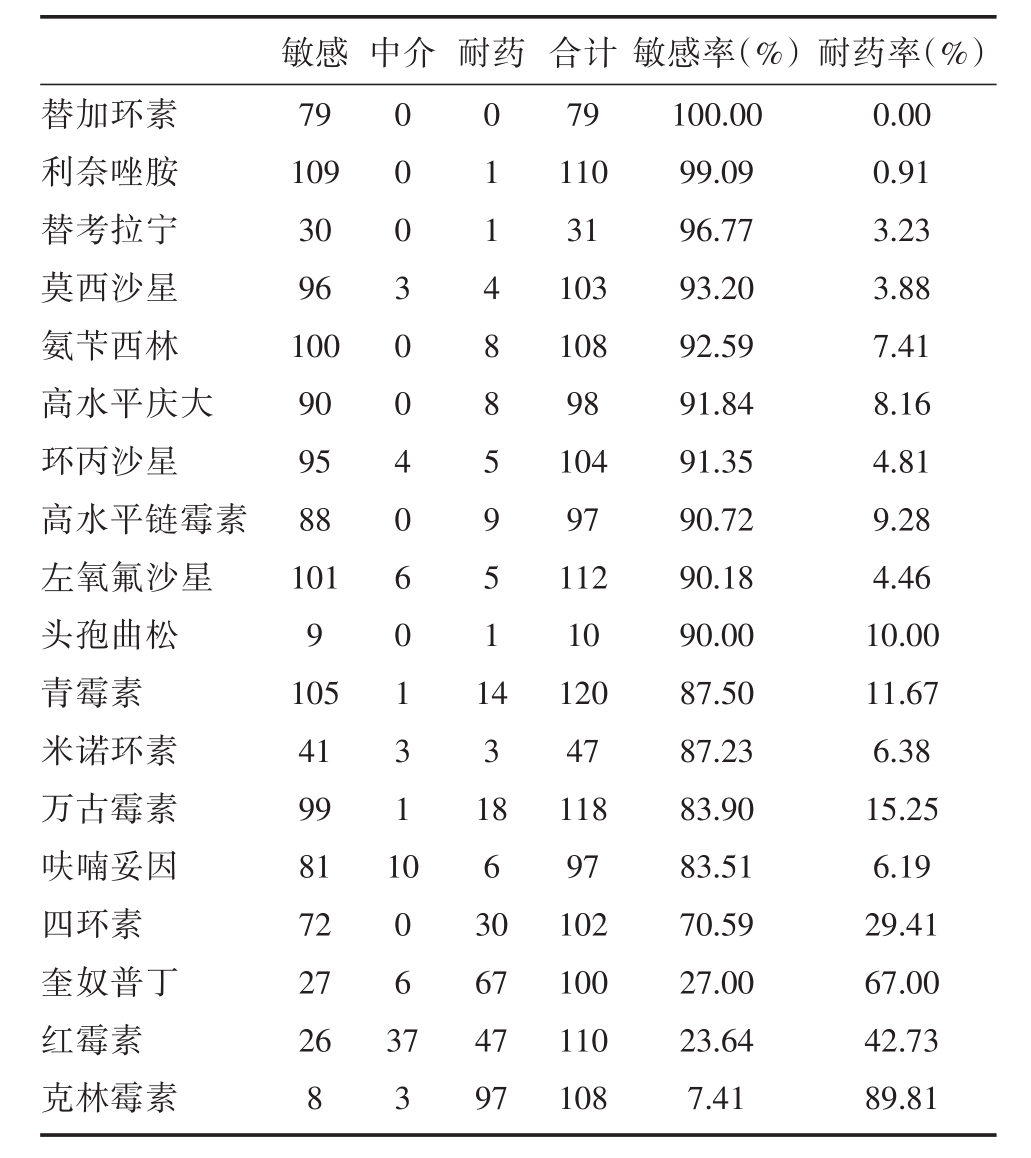
中介 耐药替加环素利奈唑胺替考拉宁莫西沙星氨苄西林高水平庆大环丙沙星高水平链霉素左氧氟沙星头孢曲松青霉素米诺环素万古霉素呋喃妥因四环素奎奴普丁红霉素克林霉素敏感79 109 30 96 100 90 95 88 101 9 105 41 99 81 72 27 26 8 0 0 0 3 0 0 4 0 6 0 1 3 1 1 0 1 1 4 8 8 5 9 5 1 1 4 3 1 0 0 6 3 8 6 3 0 7 3 67 47 97合计79 110 31 103 108 98 104 97 112 10 120 47 118 97 102 100 110 108敏感率(%)100.00 99.09 96.77 93.20 92.59 91.84 91.35 90.72 90.18 90.00 87.50 87.23 83.90 83.51 70.59 27.00 23.64 7.41耐药率(%)0.00 0.91 3.23 3.88 7.41 8.16 4.81 9.28 4.46 10.00 11.67 6.38 15.25 6.19 29.41 67.00 42.73 89.81
3 讨论
急性胆管炎发生在感染的,通常阻塞的胆道系统,最常见的阻塞原因是结石。胆道内到全身循环的细菌感染被认为是胆管炎中菌血症和败血症发生的主要病因。急性胆管炎发病的主要因素是胆道梗阻、腔内压增高和胆汁感染。胆汁通常是无菌的,感染的途径可能是直接的、血行的或淋巴管。由于胆道梗阻,胃肠道内没有胆汁和分泌IgA,导致细菌菌群的改变、粘膜完整性的丧失、内毒素灭活和促进细菌过度生长、门静脉菌血症、内毒素血症以及内毒素(LPS)向肝脏易位,导致脓毒症[4,5]。入侵胆道内的细菌多来源于肠内,但实际的情况因地区、时间差异不同可能存在一定变化[6,7]。因此,最新的指南[3,8]指出,参考所在地区或区域近期致病菌及其耐药情况、抗菌药物在胆汁中的浓度及时尽早的使用经验性的抗菌药物是较为关键的治疗措施之一。
本研究中急性胆管炎胆汁中细菌培养的阳性率为82.80%,这与国外研究[3]指出的急性胆管炎胆汁细菌培养阳性率为28%~93%相符合。而与国内多个研究有关胆道感染胆汁中细菌培养阳性率及细菌构成上均有所不同,如梁伟潮等研究[9]报道广州佛山地区胆道感染患者胆汁培养阳性率高达87.64%,邹雪飞等研究[10]报道滨州市区胆道感染患者胆汁培养阳性率75.3%,李平等研究则发现重庆市区胆道感染患者胆汁培养阳性率63.33%[11],陈海川等[12]报道南京地区的74.78%。这应该与疾病的诊断标准相关,地区差异,抗菌素的应用习惯不同等因素相关。本研究中急性胆管炎胆汁培养中以革兰氏阴性菌为主占64.25%,革兰氏阳性菌占34.08%,前五位细菌分别为大肠埃希菌129例(36.0%)、粪肠球菌59例(16.5%)、铜绿假单胞菌27例(7.5%)、肺炎克雷伯菌肺炎亚种24例(6.7%)以及屎肠球菌17例(4.7%)这与国内文献[13,14]报道胆道感染细菌培养前三位分别为大肠埃希菌、肺炎克雷伯菌和粪肠球菌,和赵嘉美等研究[15]报道胆道感染患者胆汁培养前三位分别为大肠埃希菌、肺炎克雷伯菌和铜绿假单胞菌均存在一定差异。
除此之外,随着广谱抗生素的广泛使用,同一细菌的耐药性在不同国家、不同地区、不同器官、不同疾病也存在一定差异,同时目前的研究尚未发现哪一类抗菌药物可以作为急性胆管炎经验性抗菌治疗的最佳方案,因此本地区甚至本医院或本科室细菌药敏系统的建立尤为重要。
在本次研究中发现本地区急性胆管炎患者胆汁培养为革兰氏阴性细菌中,最为敏感的药物依次为厄他培南、阿米卡星、亚胺培南、妥布霉素(耐药率小于10%),而头孢呋辛、氨苄西林、头孢唑林、头孢曲松耐药率均高于50%。一些研究[16,17]显示胆道培养革兰阳性菌对万古霉素、替考拉宁及利奈唑胺的敏感率较高,但对莫西沙星、氨苄西林、呋喃妥因及环丙沙星耐药率大于40%。本次研究中发现本地区急性胆管炎感染革兰氏阳性菌对替加环素、利奈唑胺、替考拉宁、米诺环素、莫西沙星、氨苄西林、头孢曲松敏感率均高于90%,但对于克林霉、素奎奴普丁、红霉素耐药率高于40%。可以看出本地区急性胆管炎患者相较其他地区对各抗生素耐药率均较好,特别是在喹诺酮类、氨基糖苷类、青霉素类中仍具有良好的敏感性,但亦需警惕万古霉素敏感率相较于其他地区耐药情况相对较高。
由此可见,近几年来,随着广谱抗生素的广泛使用,急性胆管炎患者胆汁培养的病原学及药敏均有所变化,现状仍然是以革兰阴性菌为主,而药敏以碳氢酶烯类及氨基糖苷类相对敏感度较高,故临床上行经验性抗菌治疗时要需引起足够重视并加强管理及监控。
参考文献
[1] Kiriyama S,Kozaka K,Takada T,et al.Tokyo Guidelines 2018:diagnostic criteria and severity grading of acute cholangi-tis(with videos)[J].J Hepatobiliary Pancreat Sci,2018,25(1):17-30.
[2] 中华医学会外科学分会胆道外科学组.急性胆道系统感染的诊断和治疗指南(2011版)[J].中华消化外科杂志,2011,10(1):9-13.
[3] Gomi H,Solomkin JS,Schlossberg D,et al.Tokyo Guide-lines 2018:antimicrobial therapy for acute cholangitis and cho-lecystitis[J].J Hepatobiliary Pancreat Sci,2018,25(1):3-16.
[4] Pavlidis ET,Pavlidis TE.Pathophysiological consequences of obstructive jaundice and perioperative management[J].Hepato-biliary Pancreat Dis Int,2018,17(1):17-21.
[5] Navaneethan U,Jayanthi V,Mohan P.Pathogenesis of cholangi-tis in obstructive jaundice-revisited[J].Merva Gastroenterol Di-etol,2011,57(1):97-104.
[6] Tang R,Wei Y,Li Y,et al.Gut microbial profile is altered in primary biliary cholangitis and partially restored after UDCA therapy[J].Gut,2018,67(3):534-541.
[7] Volta U,Caio G,Tovoli F,De Giorgio R.Gut-liver axis:an im-mune link between celiac disease and primary biliary cirrhosis[J].Expert Rev Gastroenterol Hepatol,2013,7(3):253-261.
[8] Sulzer JK,Ocuin LM.Cholangitis:Causes,Diagnosis,and Management[J].Surg Clin North Am,2019,99(2):175-184.
[9] 梁伟潮,朱应昌,韩福郎,等.胆道感染患者胆汁中病原菌的分布及对药物的敏感性变化分析[J].吉林医学,2018,39(2):301-303.
[10] 邹雪飞,吴广利,王伟,等.胆石症合并急性胆管炎患者胆汁及血液病原菌培养及药敏分析[J].中华实验和临床感染病杂志,2015,9(1):91-95.
[11] 李平,康继莲.胆石症合并胆道感染患者的病原菌分布及耐药性分析[J].检验医学与临床,2017,14(10):1451-1455.
[12] 陈海川,俞海波,肖竣,等.不同程度急性胆管炎患者的胆汁细菌培养[J].中华肝胆外科杂志,2012,10(18):740-742.
[13] 梁美春,张小娇,马建国.肝胆外科胆汁感染现状调查及胆汁细菌谱与耐药性分析[J].中国微生态学杂志,2017,29(11):1315-1318.
[14] 黄加铭,张加勤,马晓波,等.胆道感染病原菌的分布及耐药性分析[J].中华医院感染学杂志,2014,24(6):1359-1361.
[15] 赵嘉美,郭丹丹,李文利,等.胆总管结石合并感染患者鼻胆管引流前后胆汁细菌分布及其耐药性[J].中国感染控制杂志,2018,17(6):512-516.
[16] 延学军,岳风芝,赵付生,等.急性胆管炎患者胆汁病原菌分布与药敏性分析[J].中华医院感染学杂志,2016,26(6):1281-1283.
[17] Karpel E,Madej A,Bu?dak ?,et al.Bile bacterial flora and its in vitro resistance pattern in patients with acute cholangitis re-sulting from choledocholithiasis[J].Scand J Gastroenterol,2011,46(7-8):925-930.

