门诊行小儿肝穿刺活检,因患儿在清醒状态下难以配合,常需深度镇静。而肝穿刺活检操作时间短,一般在5~10分钟内完成,因此麻醉要求起效快、苏醒迅速及不良反应少[1]。丙泊酚有良好的镇静作用,目前为门诊镇静的常规用药方案,但因镇痛不佳、单纯推注丙泊酚时部分患儿有时仍会因为疼痛发生躁动,影响手术操作[2];瑞芬太尼是μ受体激动剂,为强效麻醉性镇痛药,镇痛作用强、起效快,且持续时间短。本研究旨在探讨丙泊酚复合瑞芬太尼在小儿行肝穿刺活检中应用的效果,为今后临床应用提供参考。
1 资料与方法
1.1 一般资料
经我院伦理委员会批准,拟选我院2018年10月到2019年6月期间在门诊治疗室行B超引导下肝穿刺活检的患儿40例,将病例随机分为两组:单纯丙泊酚组(A组,20例)及丙泊酚联合瑞芬太尼组(B组,20例);ASAⅠ~Ⅱ级,年龄3~12岁。排除标准:病态肥胖,有严重的先天性心肺疾病或地中海贫血等遗传病、近期有呼吸道感染、过敏体质、多动症等其他特殊病史、或因术中意外需行抢救等紧急情况而退出者。术前一天提前访视,跟患儿家属签订知情同意书,常规禁饮禁食,患者入室后按随机序列表顺序分别纳入A组及B组。
1.2 麻醉方案
术前常规禁饮禁食,入门诊治疗室(B超室)后开放静脉,行多功能监测血压(BP)、心率(HR)、呼吸频率(RR)、血氧饱和度(SpO2)等,并准备好气管插管等急救用品。患儿取仰卧位,予4~6 L/min氧流量鼻导管吸氧。A组在腹部皮肤消毒前予以2.5~3.5 mg/kg丙泊酚分次缓慢静推,尽量避免由于推注过快导致血压急剧下降或呼吸抑制。B组在消毒前予以1.5~2.5 mg/kg丙泊酚,使患儿平稳入睡,并在穿刺前予以0.5μg/kg瑞芬太尼,分次缓慢推注。待患儿睫毛反射和体动消失后实施穿刺,穿刺过程中如患儿发生躁动则再追加丙泊酚10~30 mg加深麻醉,保证穿刺顺利完成。麻醉穿刺期间如患儿SpO2低于95%,立即托下颌或经面罩给氧,必要时行人工手控辅助呼吸,使SpO2回升至99%以上再行操作。如血压、心率下降超过术前20%,可酌情使用多巴胺或阿托品维持血流动力学平稳。两组穿刺时间均在5~10 min。全部病例均未出现多次插管失败或须紧急抢救等特殊情况。
1.3 观察指标
术中持续监测并记录NⅢP(包括MAP)、心率(HR)、呼吸频率(RR)、血氧饱和度(SpO2)的变化,密切观察患儿口唇颜色及胸腹部呼吸动度。观察记录两组丙泊酚药物总量、呼吸抑制和躁动情况,比较两组术后初醒时间,评估两组穿刺成功率和安全性。
1.4 统计学分析
根据前期19例预实验结果,录入各组PaO2均数及标准差,将检验水准α设置为0.05,检验效能(1-β)设为80%,采用PASS软件(NCSS,USA)计算样本量,结果提示每组病例数不少于16个为宜。考虑到研究脱漏,遂额外增加20%样本量。试验先后招募病例47个,最终符合入组的样本量为40例,每组平均20例。统计分析采用SPSS 22.0统计学软件进行统计学处理。计量资料以“均数±标准差”表示,组内比较采用方差分析。各组间比较主要采用t检验,计数资料采用χ2检验,P<0.05为差异具有统计学意义。
2 结 果
2.1 两组患儿一般情况比较(见表1)
一般情况组间差异无统计学意义(P>0.05),说明两组具有可比性。
表1 两组患儿一般资料比较

组别A组B组男/女/例11/9 10/10年龄/岁6.2±2.6 6.5±2.0体重/kg 26.3±8.1 28.2±6.6 ASA分级(Ⅰ/Ⅱ)/例7/13 8/12
2.2 两组不同时间点MAP、HR及SpO2变化(见表2)
A组在T1、T2时刻血压下降,与T0相比有统计学差异(P<0.05);两组间同时刻点相比HR、SpO2无明显差异(P>0.05),说明B组血流动力学更平稳。
表2 两组患者MAP、HR、Sp O2麻醉前、后的变化
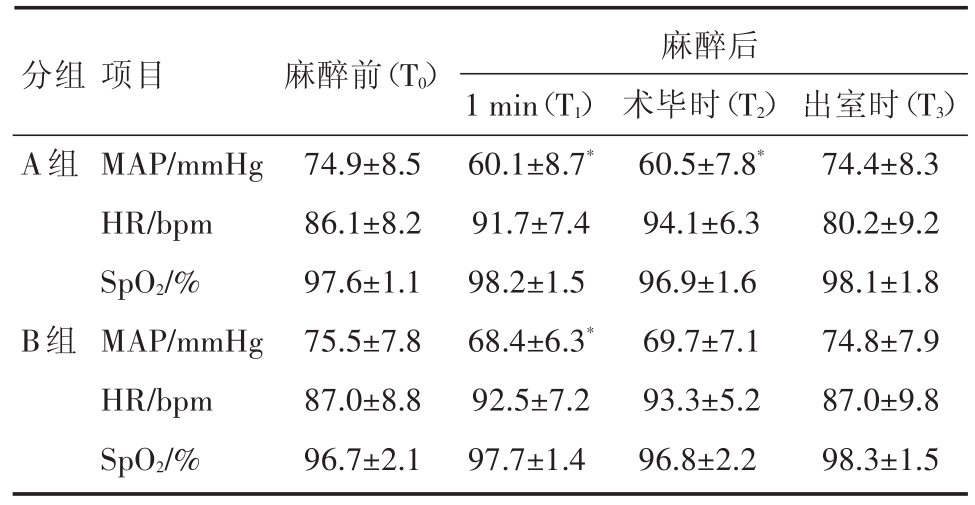
注:*与麻醉前比较,P<0.05
分组A组麻醉后B组项目MAP/mmHg HR/bpm SpO2/%MAP/mmHg HR/bpm SpO2/%麻醉前(T0)74.9±8.5 86.1±8.2 97.6±1.1 75.5±7.8 87.0±8.8 96.7±2.1 1 min(T1)60.1±8.7*91.7±7.4 98.2±1.5 68.4±6.3*92.5±7.2 97.7±1.4术毕时(T2)60.5±7.8*94.1±6.3 96.9±1.6 69.7±7.1 93.3±5.2 96.8±2.2出室时(T3)74.4±8.3 80.2±9.2 98.1±1.8 74.8±7.9 87.0±9.8 98.3±1.5
2.3 两组丙泊酚总量、呼吸抑制率、躁动发生率和初醒时间比较(见表3)
丙泊酚总量、躁动发生率和初醒时间A组皆大于B组(P<0.05),而呼吸抑制率两组无明显差异(P>0.05)。说明B组联合使用瑞芬太尼后,可以减少患儿术中躁动,加快苏醒,且并不增加呼吸抑制风险。
表3 两组患者丙泊酚用量、呼吸抑制率、躁动发生率、初醒时间比较
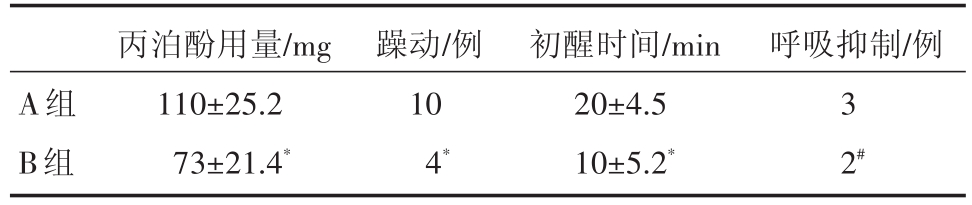
注:与A组比较,*P<0.05,#P>0.05
A组B组丙泊酚用量/mg 110±25.2 73±21.4*躁动/例10呼吸抑制/例3 4*初醒时间/min 20±4.5 10±5.2*2#
3 讨论
随着儿科诊疗技术的不断提高,目前小儿肝穿刺活检在门诊治疗室开展日渐增多,一般须在B超引导下精确操作。由于肝穿刺操作时间短,而刺激强度并不小,加上小儿容易紧张或恐惧,自控能力较差,因此常需辅以适当的全麻镇静以保证穿刺的顺利进行[3,4]。鉴于门诊监测和急救设备不全,门诊麻醉一般采用“单一用药”原则,目前常用方案为丙泊酚静脉全麻[5]。丙泊酚起效快、苏醒迅速,镇静作用强大,而镇痛不佳,很多时候均未能消除疼痛应激,部分患儿会因疼痛而躁动,从而影响穿刺操作。这时为消除患儿躁动则需立即追加丙泊酚以加深麻醉,当剂量过大或推注过快时,又会对循环、呼吸功能造成明显抑制[6]。因此,单纯镇静对此类操作的效果并不十分理想,镇静复合短效镇痛的方案可能更为有利。
目前有研究表明在小儿胃肠镜检查和小儿ERCP术中采用丙泊酚联合芬太尼麻醉效果比单纯丙泊酚为好,但芬太尼作用时间长,可能存在迟发性呼吸抑制,对短小手术如肝穿刺活检优势并不明显[7,8]。与芬太尼相比,瑞芬太尼起效更快,作用持续时间更短,是真正的短效强力镇痛药。但由于瑞芬太尼多用于持续泵注给药,在门诊静注用于小儿镇痛的剂量和速度尚无统一标准,在复合丙泊酚使用时、如剂量过大则容易导致呼吸抑制等风险,因此在门诊操作的应用尚存争议[9]。
研究表明,异丙酚和瑞芬太尼的推荐浓度取决于手术类型、手术刺激程度、局部麻醉阻滞的使用以及患者的通气状态[6,7]。本研究在小儿门诊肝穿刺活检手术中分别采用单纯丙泊酚静注和丙泊酚复合小剂量瑞芬太尼静注,以比较两种麻醉方案的效果和安全性。在预实验中,我们分别采用了0.2μg/kg、0.5μg/kg、1.0μg/kg的瑞芬进行观察,发现0.5μg/kg剂量的瑞芬太尼既可以起到良好的镇痛效果,又不会对呼吸、循环造成明显的抑制,因此我们选定的这个剂量的方案进行研究。我们发现B组复合0.5μg/kg的瑞芬太尼后,丙泊酚总量和躁动发生率明显减少,麻醉效果满意,血流动力学更平稳,患儿苏醒更快,且并不增加呼吸抑制风险。我们分析,这可能因为A组使用单一丙泊酚镇静,未能阻断疼痛应激,在患儿发生躁动后又需追加较多丙泊酚,因此反而不利于血流动力学平稳,影响总体麻醉效果。值得注意的是,丙泊酚本身对循环、呼吸系统的抑制较轻且多为一过性,一般认为与药物剂量和给药速度有关,通过调整给药方案可以缓解;而在复合使用瑞芬太尼时,应注意避免两种药物同时达到药效高峰,以免增加呼吸抑制风险[10]。本研究不足之处在于:①门诊行肝穿刺的患儿自身基础病不尽相同,其中常见疾病包括白血病、地中海贫血、肝肿物等,且年纪跨度较大(3~12岁),因此患儿本身对麻醉的耐受能力并不一致;②麻醉给药方式差异,由于门诊缺乏泵注仪器,只能采用手动缓慢推注,这就容易导致给药速度不均衡;③穿刺医生不同,肝穿刺活检看似简单,但要做到精准、迅速、轻柔并不容易,由于患儿基础疾病不同,甚至来自不同科室,因此负责穿刺操作的临床医生、超声医生也都不固定。因此,后续研究应尽可能选择同类患儿、同一手术操作医生,匀速的给药设备,则研究结果将更有说服力。
综上所述,对门诊小儿肝穿刺活检、采用丙泊酚联合小剂量瑞芬太尼能改善麻醉效果,减轻不良反应,加快苏醒,使麻醉和手术过程更平稳。因此丙泊酚联合小剂量瑞芬太尼在小儿肝穿刺活检中具有积极的应用价值。
参考文献
[1] Seol TK,Lim JK,Yoo EK,et al.Propofol-ketamine or propofolremifentanil for deep sedation and analgesia in pediatric patients undergoing burn dressing changes:a randomized clinical trial[J].Paediatr Anaesth,2015,25(6):560-566.
[2] 符永强,徐彩萍.瑞芬太尼静脉输注联合丙泊酚靶控输注和七氟烷吸入麻醉在小儿短小手术中的效果[J].海峡药学,2017,29(12):127-129.
[3] Amaral JG,Schwartz J,Chait P,et al.Sonographically guided percutaneous liver biopsy in infants:a retrospective review[J].AJR Am JRoentgenol,2006,187(6):W644-649.
[4] An LJ,Zhang Y,Su Z,et al.A single dose of dezocine suppresses emergence agitation in preschool children anesthetized with sevoflurane-remifentanil[J].BMC Anesthesiol,2017,17(1):154.
[5] Khurmi N,Patel P,Kraus M,et al.Pharmacologic considerations for pediatric sedation and anesthesia outside the operating room:a review for anesthesia and non-anesthesia providers[J].Paediatr Drugs,2017,19(5):435-446.
[6] Karacaer F,Biricik E,Ilginel M,et al.Remifentanil-ketamine vs.propofol-ketamine for sedation in pediatric patients undergoing colonoscopy:A randomized clinical trial[J].Rev Bras Anestesiol,2018,68(6):597-604.
[7] Abu-Shahwan I,Mack D.Propofol and remifentanil for deep sedation in children undergoing gastrointestinal endoscopy[J].PaediatrAnaesth,2007,17(5):46460-3.
[8] 沙瑾.丙泊酚联合芬太尼静脉麻醉在小儿ERCP术中的应用[J].现代消化及介入诊疗,2013,18(1):30-31.
[9] Anderson BJ,Bagshaw O.Practicalities of total intravenous anesthesia and target-controlled infusion in children[J].Anesthesiology,2019,131(1):164-185.
[10]Bagshaw O.Pediatric anesthesia editorial-propofol and remifentanil:to mix or not to mix[J].Paediatr Anaesth,2016,26(7):677-679.

