胆囊结石伴胆总管结石的传统行开腹胆囊切除、胆总管取石T管引流术中,胆道探子或取石钳探查胆管、取石的盲目性较大,容易造成胆道损伤且结石难以保证取除干净;放置T管引流虽然可以减轻胆管炎症反应、便于术后经T造影评估术后胆道情况、经该隧道取残石等,但这样容易造成胆汁丢失,导致消化不良和电解质紊乱,以及患者较长时间带造成生活不便,甚至感染[1,2]。笔者收集2017年1月至2019年1月24例胆囊结石合并胆总管结石患者行腹腔镜胆囊切除及胆总管探查,术中应用超声和胆道镜并行胆总管一期缝合,取得良好的治疗效果,现将病例资料进行回顾和总结,报道如下。
1 临床资料
1.1 一般资料
24例患者男性13例,女性11例,年龄26~79岁。临床有腹痛、或伴畏寒、发热、黄疸等胆石症表现,患者术前均行肝胆胰脾超声或腹部CT,部分病例行MRCP检查,21例术前临床检查资料评估有胆总管结石,其中有3例术前影像学见胆总管稍扩张、未见明确结石,术前评估心肺功能能耐受手术,无绝对手术禁忌证,见表1。
1.2 方法
所有患者均采用气管插管全身麻醉,麻醉起效后,常规消毒铺巾后,在脐部下缘取约1.2 cm切口,建立气腹和观察孔,在剑突下取1.2 cm及右肋下0.5 cm作为操作孔,根据术中操作情况需要可以增加操作孔,观察孔置入腹腔镜,操作孔置入腹腔镜器械,先探查腹腔,无损伤钳提起胆囊,暴露肝门区,腹腔镜超声探查胆囊三角,明确胆囊管、胆总管、肝总管、左右肝管病变情况,明确结石位置大小等,用电钩或超声刀切开胆囊三角区系膜,分离出胆囊管,结扎胆囊管,顺行切除胆囊,若胆囊三角解剖不清或粘连严重,为了避免胆总管或右肝管损伤可采用逆行切除胆囊(亦可先结扎胆囊管暂不切除胆囊,可以提拉胆囊暴露胆总管,最后才切除胆囊),用超声再次明确胆总管、门静脉情况、在胆总管前壁用5-0细针带电凝纵行切开约1 cm,插入胆道镜探查胆总管、肝总管和左、右肝管,用套石篮取石、石头较大可以用液电碎石或适当延伸胆管切口取石,对于细小结石用导尿管(F8-12)反复冲洗出胆管,最后用胆道镜仔细检查胆管,确保胆管内无结石残留、十二指肠乳头张开闭合功能良好后,用5-0 PDS可吸收无损伤缝线连续或间断胆管壁全层缝合,再用超声探查,评估胆总管缝合效果,这样可以防止胆道狭窄或前后壁被缝合,置小网膜孔腹腔引流管,典型病例见图1。
表1 患者术前基本情况
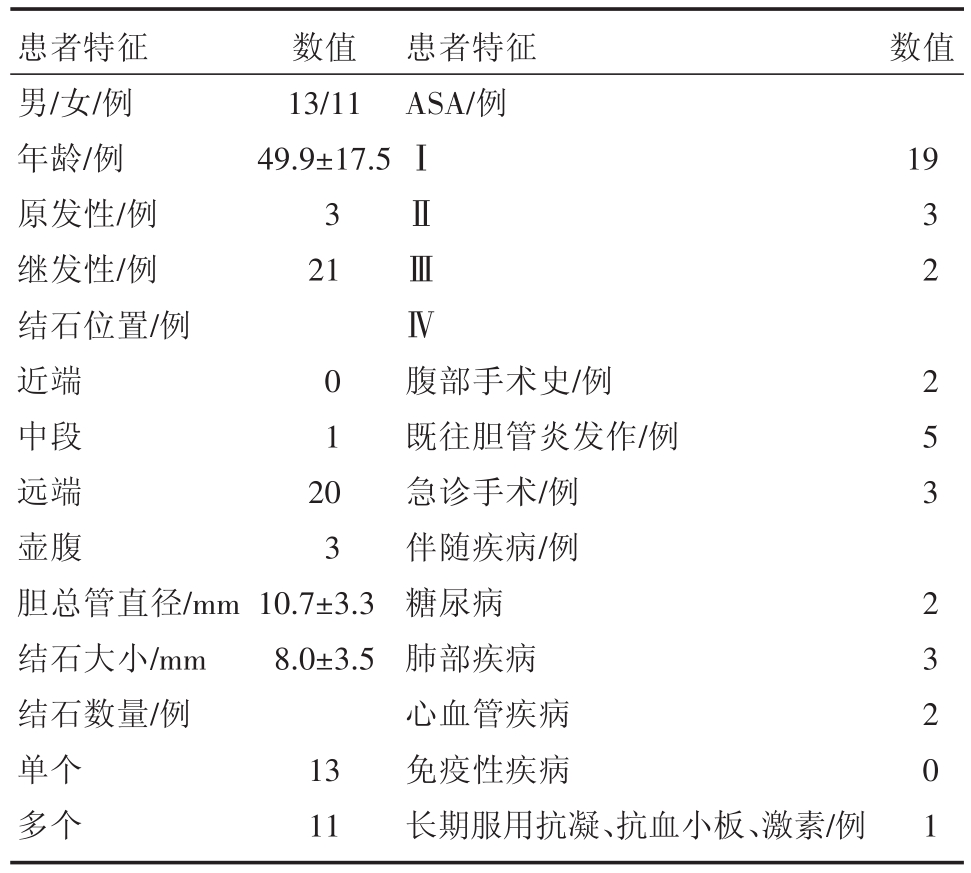
患者特征男/女/例年龄/例原发性/例继发性/例结石位置/例近端中段远端壶腹胆总管直径/mm结石大小/mm结石数量/例单个多个数值13/11 49.9±17.5 3 21患者特征ASA/例数值ⅠⅡⅢⅣ19 0 1 20 3 10.7±3.3 8.0±3.5 13 11腹部手术史/例既往胆管炎发作/例急诊手术/例伴随疾病/例糖尿病肺部疾病心血管疾病免疫性疾病长期服用抗凝、抗血小板、激素/例3 2 2 5 3 2 3 2 0 1
2 结果
24例临床病例均获得手术成功,术前未发现结石而在手术中腹腔镜超声发现、胆道镜确诊胆总管结石3例(3/24),结石均位于胆总管下端、直径大小约5~7 mm,有腹腔粘连2例,需要耐心分离,可以利用术中超声了解血管、胆管等重要组织情况,较少损伤,术中有3例套石篮取石困难、需要液电碎石,胆总管切开范围一般1~1.5 cm,根据术前评估结石大小决定切开大小,平均手术时间101.3±15.9 min,平均失血量13.4 ±3.4 mL,平均拔除引流管时间5.5±1.1 d,平均住院时间11.2±4.0 d,其中3例出现引流液为含胆汁样液,保持通畅引流畅通至引流量逐渐减少至5 mL以下约5~7 d拔除引流管,24例患者均顺利出院,出院后随访1~6个月,均未出现明显并发症,复查B超、CT或MR未发现胆总管结石复发及狭窄情况。
3 讨论
随着腹腔镜技术不断发展,对于胆囊结石合并胆总管结石的患者,腹腔镜胆囊切除胆总管探查术在临床上得予开展,其创口小、恢复快、甚至可以免带T管等优势得到广泛应用[3-5]。但胆道系统变异情况多,总变异率为42.3%,其中解剖变异占到了41%,肝外胆道变异也有8.8%[6-8],加之腹腔镜手术过程中术者无法用手触摸腹腔内的胆囊、肝管、胆总管等组织器官,在进行胆囊三角的分离、胆总管的切开探查等操作时,若胆道、血管变异,尤其在组织水肿、粘连等,极其容易造成胆道损伤[9,10]。即使由经验丰富的术者操作,在腹腔镜胆囊切除胆总管探查手术中,胆道损伤仍时有发生,国内外报道,胆管损伤的发生率为0.5%~1.6%左右[11-14]。胆管一旦损伤处理较为棘手,再次手术率高,预后多较差[15,16]。
而腹腔镜术中超声与普通超声相比,可以避免腹壁、肠管等干扰,直接紧贴脏器,能够清晰显现胆总管、肝总管、左右肝管、胆囊管、门静脉等,在手术操作过程中可以起到导航作用,可重复性好,没有辐射,可以减少术中胆道损伤[17-18]。腹腔镜超声可以发现胆囊管结石、胆总管结石,帮助术中决定手术策略。虽然胆道造影能够显现胆道情况,但是胆道造影需要插管操作,可能造成胆管损伤,需要专门的放射科医师的协助参与,重复操作显得十分繁琐,具有辐射性,若有造影剂渗漏可能影响胆道造影效果[19]。
本研究分析总结我院24例患者胆囊结石合并胆总管结石行术中超声联合胆道镜在腹腔镜胆总管一期缝合,术中发现胆总管结石3例(3/24),术前检查B超、CT或MRCP未发现,这样可以一次手术一并处理胆总管结石,避免二期手术处理,应用术中超声可以比经腹更直接评估胆道结石大小、位置、数量等。胆总管主要为继发性结石、下端为多见,在切开胆总管时,可以用5-0小针带电凝切开胆总管、这样尽量少损伤胆管壁,再用胆道镜直视下取石,并充分观察十二指肠乳头功能情况,若功能良好、无狭窄,可以用5-0或6-0单股可吸收线连续或间断全层外翻缝合,针距1 mm,边距1~1.5 mm为宜,缝合应均匀、无张力、密度适当、无渗漏,避免术后胆道狭窄,吸引器吸净周围积液、纱块再蘸干,用干净纱块覆盖胆总管,纱块有无黄染,观察有无胆漏,最后再用超声观察胆总管缝合连续性情况,避免缝合不当造成胆道狭窄、前后壁误缝,最后放置引流管,位置一定要放好,一旦有少量胆漏可以通过充分引流基本能痊愈,避免再次手术。这样可以免除胆总管放置T管,加快病人康复,明显提高这些患者生活质量。
然而在施行该术式时,需要严格把握适应症,让患者最大获益。笔者总结临床经验及相关文献报道[20-22],胆总管一期缝合适应证主要有:①胆总管要扩张8 mm以上,胆道镜能进入胆管,这样既能取净结石又避免术后胆管狭窄;②单纯的肝外胆管结石而不合并肝内胆管结石并能够确保取净结石,可以一期缝合,而对于合并肝内胆管结石一般难以保证取净,不建议一期缝合;③胆道镜下能够确认结石无残留并且十二指肠乳头开闭功能良好;④胆总管壁缝合均匀、确切可靠,无胆漏、无狭窄。
综上所述,腹腔镜术中超声联合胆道镜保证胆总管一期缝合安全有效,该术式创伤小、恢复快,但需要选择病例。
参考文献
[1] 曾天才,陈先祥,徐阳,等.腹腔镜胆总管探查内支架引流及T管引流治疗肝外胆管结石的临床研究[J].中国普外基础与临床杂志,2014,21(10):1203-1206.
[2] 张宗明,苑海明,张翀.双镜联合同期治疗胆囊结石合并胆总管结石的策略[J].中华消化外科杂志,2015,14(4):280-283.
[3] 管辉球,景岚,徐锁青,等.胆总管一期缝合经胆囊管胆管引流与鼻胆管引流的对比研究[J].中华外科杂志,2018,56(2):130-134.
[4] 殷子,徐康,孙健,等.腹腔镜胆总管探查取石术后一期缝合与T管引流随机对照试验的系统评价和meta-分析[J].岭南现代临床外科,2016,16(6):404-412.
[5] Khaled YS,Malde DJ,de Souza C,et al.Laparoscopic bile ductexploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis[J].Surg Endosc,2013,27(11):4164-4170.
[6] 谢英园,罗世云,夏中平,等.腹腔镜切除冰冻Calot三角的胆囊临床体会[J].肝胆胰外科杂志,2015,27(1):58-59.
[7] Wu JS,Peng C,Mao XH,Lv P.Bile duct injuries associated with laparoscopic and open cholecystectomy:sixteen-year experience[J].World JGastroenterol,2007,13(16):2374-2378.
[8] Kerimoglu RS,Bostanci EB,Dalgic T,et al.Management of laparoscopic cholecystectomy-related bile duct injuries:a tertiary center experience[J].Arch Iran Med,2017,20(8):487-493.
[9] Araki K,Conrad C.Intraoperative laparoscopic ultrasound for laparoscopic hepatopancreatobiliary surgery//Laparoscopic Liver,Pancreas,and Biliary Surgery[M].John Wiley&Sons,Ltd,2016
[10]邱枫,刘佐军,孙海涛,等.继发性胆总管结石外科治疗中应用腹腔镜超声的优势[J].中华肝胆外科杂志,2017,23(11):766-770.
[11]罗飞.腹腔镜胆囊切除术中胆道造影的临床应用[J].中国现代普通外科进展,2015,18(6):469-470.
[12]顾兴伟,金荣.腹腔镜胆囊切除术中胆道造影100例临床分析[J].腹腔镜外科杂志,2015,20(12):931-933.
[13]杨志勇,吴永哲,崔宏力,等.选择性经胆囊管胆道造影在急诊腹腔镜胆囊切除术中的应用[J].中国医药导报,2017,14(8):111-114.
[14]Hogan NM,Dorcaratto D,Hogan AM,et al.Iatrogenic common bile duct injuries:Increasing complexity in the laparoscopic era:A prospective cohort study[J].Int JSurg,2016,33 Pt A:151-156.
[15]李明皓,杨志琦,刘晶,等.腹腔镜胆囊切除术中胆管损伤处理30例临床分析[J].中华普通外科杂志,2017,32(8):670-673.
[16]崔宏力,周长宇,刘建东,等.腹腔镜胆囊切除术后胆总管残余结石的危险因素分析[J].国际外科学杂志,2014,41(11):758-762.
[17]中国肝胆外科术中超声学院.腹腔镜超声在肝脏外科的应用专家共识(2017)[J].中华肝胆外科杂志,2017,23(11):721-728.
[18]Jamal KN,Smith H,Ratnasingham K,et al.Meta-analysis of the diagnostic accuracy of laparoscopic ultrasonography and intraoperative cholangiography in detection of common bile duct stones[J].Ann R Coll Surg Engl,2016,98(4):244-249.
[19]Falcone RA,Fegelman EJ,Nussbaum MS,et al.A prospective comparison of laparoscopic ultrasound vs intraoperative cholangiogram during laparoscopic cholecystectomy [J].Surg Endosc,1999,13(8):784-788.
[20]汤晓东,刘双海,蒋剑,等.不同方式腹腔镜胆道探查术治疗肝外胆管结石的临床研究[J].中华肝胆外科杂志,2013,19(8):589-592.
[21]高飞,芦小龙,李剑辉,等.两种微创术式治疗胆囊结石合并胆总管结石的效果比较[J].临床肝胆病杂志,2017,33(2):300-303.
[22]杨彦,张剑,楼健颖,等.腔镜胆总管探查取石免留置鼻胆管引流一期缝合术临床疗效的多中心回顾性研究(附312例报告)[J].中华消化外科杂志,2018,17(1):68-74.

