

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 93-97.DOI: 10.3969/j.issn.1009-976X.2020.01.021
摘要:
近年来,随着喉内显微技术的快速发展,支撑喉镜下处理患者喉部病变已成为常用手段,虽然其具有操作简单、术后并发症少等优势,但仍有部分患者因术中声门区病变暴露困难而影响手术效果,甚至导致手术无法进行。因此,支撑喉镜下行喉部手术前分析患者声门暴露程度对手术顺利进行至关重要。由于患者头颈部解剖结构各有不同,术中声门区暴露情况也有所不同[1]。因此,本研究通过收集210例在支撑喉镜下行喉部手术患者临床资料,并分析其与声门区暴露情况关系,以确保患者手术顺利完成。详细结果如下。
选取2017年5月~2018年10月医院收治的210例在支撑喉镜下行喉部手术患者作为受试对象。入选标准:①年龄>18周岁;②均自愿加入本研究;③无颈部肿瘤放疗、颈部手术和创伤史者。排除标准:①有严重颈部感染及颈部活动受限者;②有沟通障碍者;③颞颌关节紊乱、口腔或下颌骨畸形患者;④妊娠或哺乳期女性。210例患者中有男性77例,女性133例;年龄21~71岁,平均年龄(46.83±14.07)岁;声带息肉104例,声带囊肿38例,声带结节53例,声带任克氏水肿15例。
1.2.1 资料收集 在支撑喉镜下行喉部手术前,收集所有受试者临床资料,并建立数据库,对可能影响术中声门区暴露困难的因素进行详细记录。影响因素主要有以下几方面:性别、年龄、体质指数(body mass index,BMI)、颈围、改良 Mallampati分级、下颌骨甲状软骨间夹角(thyroid-mandible an-gel,TMA)、张口度、颈部屈伸度、舌颏距(hyoid-mental distance,HMD)、胸颏距(sternum-mental dis-tance,SMD)、甲 颏 距(thyroid-mental distance,TMD)、垂直甲颏距(vertical thyroid-mental dis-tance,VTMD)、水平甲颏距(horizontal thyroid-men-tal distance,HTMD)。颈围:一般是测量喉结节点的颈部水平周长。改良Mallampati分级情况[2]:患者蹲坐,受试者伸舌至自身最大限度,按检查医师观察到咽部结构情况进行分级,可观察到咽腭弓、软腭及悬雍垂,即为1级;可观察到咽腭弓、软腭,但悬雍垂仅部分可见,即为2级;仅可观察到软腭,即为3级;未观察到软腭,即为4级。张口度:受试者最大张口时上下门齿间距离。HMD[3]:即舌骨至下颌骨颏隆凸距离;SMD[3]:即胸骨上窝至颏隆凸的距离;TMD[3]:即甲状软骨上切迹与下颌骨颏隆凸距离;VTMD[3]:即甲状软骨上切迹与颏隆凸的垂直距离;HTMD[3]:即甲状软骨上切迹与颏隆凸的水平距离。TMA[4]:指后仰位时下颌骨下缘与经甲状软骨切迹的颈部皮肤轮廓线之间的夹角。颈部屈伸度(Wilson法)[5]:使患者头部后仰至最大限度后,再嘱患者做最大限度屈颈,头颈屈伸度为此时头颈部活动角度。
1.2.2 手术方法 受试者取仰卧位后,行气管插管静脉复合全身麻醉,当肌肉处于完全松弛状态时,在支撑喉镜下观察术中声门区暴露程度,所有受试者手术均由同组经验丰富医师完成。本研究受试者均采用由桐庐南宇医疗器械厂生产的支撑喉镜(ZC型号)进行手术,避免因支撑喉镜因素影响声门区暴露程度。
1.2.3 术中声门区暴露分级 采用Cormack-Le-hane分级方法[6]:支撑喉镜下声门区可完全暴露,即为1级;支撑喉镜下仅暴露声门后联合,前联合在助手帮助下可窥及,即为2级;支撑喉镜下仅暴露会厌,前联合未窥及,即为3级;支撑喉镜下未暴露任何喉部结构,即为4级。本研究将1级、2级作为非声门区暴露困难组(113例),3级、4级作为声门区暴露困难组(97例)[3,7]。
所有受试者数据均采用SPSS 18.0处理,计数资料采用%描述,行χ2检验;计量资料采用x±s描述,行t检验;术中声门区暴露困难的多因素分析采用Logistic回归分析;采用ROC曲线分析独立危险因素指标对声门区暴露困难的诊断效能,均以P<0.05表示差异有统计学意义。
由表1可以看出,210例患者中有51例声门区可完全暴露;62例声门区后联合可清晰窥及,而前联合需经压喉后才能窥及;70例术中仅暴露会厌;27例支撑喉镜下未窥及声门区任何结构。
表1 210例患者术中声门区暴露分级情况[n(%)]

组别非声门区暴露困难组1级2级声门区暴露困难组3级4级例数 男性 女性51 62 22(43.1)30(48.4)29(56.9)32(51.6)70 27 26(37.1)14(51.9)44(62.9)13(48.1)
由表2单因素分析结果可知,性别、改良Mal-lampati分级、年龄、BMI、SMD均与术中声门区暴露困难无关(P>0.05),颈围、TMA、张口度、颈部屈伸度、HMD、TMD、VTMD、HTMD均与术中声门区暴露困难有关(P<0.05)。
表2 影响术中声门区暴露困难的logistics单因素分析
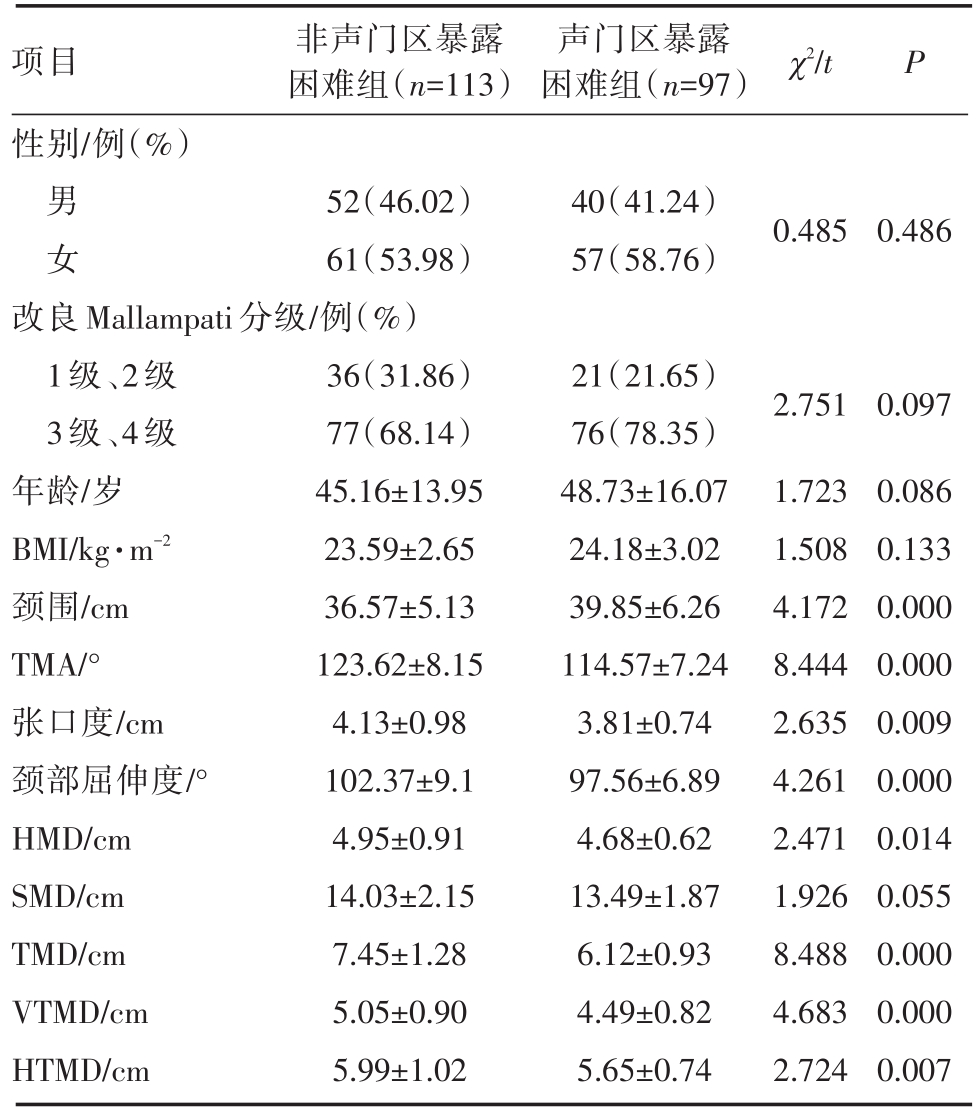
项目性别/例(%)非声门区暴露困难组(n=113)声门区暴露困难组(n=97) χ2/t P男女52(46.02)61(53.98)40(41.24)57(58.76)0.4850.486改良Mallampati分级/例(%)1级、2级3级、4级年龄/岁BMI/kg·m-2颈围/cm TMA/°张口度/cm颈部屈伸度/°HMD/cm SMD/cm TMD/cm VTMD/cm HTMD/cm 36(31.86)77(68.14)45.16±13.95 23.59±2.65 36.57±5.13 123.62±8.15 4.13±0.98 102.37±9.1 4.95±0.91 14.03±2.15 7.45±1.28 5.05±0.90 5.99±1.02 21(21.65)76(78.35)48.73±16.07 24.18±3.02 39.85±6.26 114.57±7.24 3.81±0.74 97.56±6.89 4.68±0.62 13.49±1.87 6.12±0.93 4.49±0.82 5.65±0.74 2.751 1.723 1.508 4.172 8.444 2.635 4.261 2.471 1.926 8.488 4.683 2.724 0.097 0.086 0.133 0.000 0.000 0.009 0.000 0.014 0.055 0.000 0.000 0.007
为排除上述各因素之间的相互影响,将单因素分析中有统计学意义及专业上有意义的变量(颈围、TMA、张口度、颈部屈伸度、HMD、TMD、VTMD、HTMD)纳入多因素logistic回归分析。由表3回归分析结果可知,TMA、颈部屈伸度与TMD均是影响术中声门区暴露困难的独立危险因素(P<0.05),而颈围、张口度、HMD、VTMD、HTMD尚不能作为影响支撑喉镜声门暴露的独立因素,颈围、张口度、HMD、VTMD、HTMD与声门区的暴露独立相关。行Hosmer-Lemeshow检验结果为:χ2=8.012,P=0.432,即无统计学意义,说明数据拟合较好,即该logistic回归的拟合优度较好。
根据多因素logistic回归分析结果,采用ROC曲线研究3个独立危险指标(TMA、颈部屈伸度与TMD)的诊断价值,以期望能在术前根据相关指标进行声门区暴露困难的预测。研究结果表明,TMA、颈部屈伸度与TMD的AUC(曲线下面积)均>0.7,根据ROC曲线对应的坐标点,结合最大约登指数,找出最佳分割点。结果显示,TMA对应的分割点位置为117°,即≤117°被预测为声门区暴露困难,预测灵敏度为88.5%,特异度为57.7%。TMD对应的分割点位置为6.5,即6.5被预测为声门区暴露困难,预测灵敏度为87.6%,特异度为55.7%;颈部曲伸度对应的分割点位置为100.5°,即100.5°被预测为声门区暴露困难,预测灵敏度为66.4%,特异度为71.1%。结果见表4。
表3 影响术中声门区暴露困难的logistics多因素分析结果

变量TMA颈部屈伸度TMD颈围张口度HMD VTMD HTMD SMD β P 1.855 1.445 1.511-0.27 0.383 0.202 0.348 0.275 0.038 SE 0.498 0.372 0.417 0.174 0.263 0.256 0.19 0.184 0.188 wald 13.875 15.089 13.130 2.416 2.134 0.62 3.35 2.237 0.042 0.000 0.000 0.002 0.120 0.144 0.431 0.067 0.135 0.838 OR 6.393 4.243 4.533 0.764 1.467 1.223 1.416 1.316 1.039 95%CI 2.158~18.941 1.754~10.266 1.349~15.234 0.543~1.073 0.877~2.455 0.741~2.02 0.976~2.055 0.918~1.887 0.719~1.502
表4 ROC曲线分析结果及灵敏度、特异度
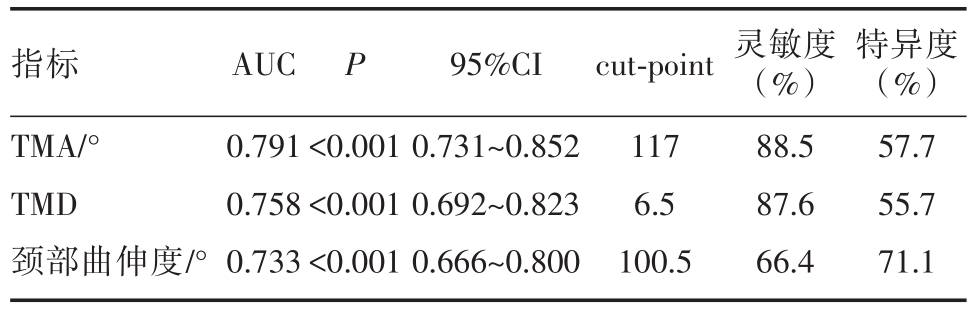
指标TMA/°TMD颈部曲伸度/°AUC 0.791 0.758 0.733 P<0.001<0.001<0.001 95%CI 0.731~0.852 0.692~0.823 0.666~0.800 cut-point 117 6.5 100.5灵敏度(%)88.5 87.6 66.4特异度(%)57.7 55.7 71.1

图1 TMA、颈部屈伸度与TMD作为诊断指标的ROC曲线
随着显微技术的广泛应用,声带良性病变及部分癌前病变患者多采用经口支撑喉镜手术进行治疗[8,9]。声带息肉、声带白斑及声带囊肿等声带疾病是耳鼻喉科常见病,其患病率呈上升趋势,已严重影响患者正常生活、工作,临床常采用支撑喉镜手术治疗。还有部分喉癌患者,将经喉外径路手术改为支撑喉镜下手术,其对术中声门区暴露情况要求更高[10]。术中声门区良好暴露有利于手术顺利进行,若术中视野暴露不佳,将可能会误伤周围其他重要器官,影响患者术后声带恢复。因此,本研究主要目的是通过术前临床相关因素对术中声门区暴露情况进行预测,以期为手术顺利进行提供帮助。
麻醉科医师最早对术中声门区暴露程度进行分级,主要依据标准为Mallampati分级,在患者全身麻醉前用于评估气管插管风险。麻醉科医师在声门区暴露后联合的情况下,即可完成麻醉插管,且随着显微技术在气管插管中的成熟应用,气管内插管在声门区暴露不佳的情况下也可顺利完成[11]。而支撑喉镜下行喉部手术对声门区暴露程度要求较严,仅暴露后联合将增加手术难度,因此麻醉科医师对声门区暴露分级情况并不完全适用于支撑喉镜下手术,仅起一定指导作用。相关研究发现[12,13],声门区暴露不佳患者,支撑喉镜术中长久挤压舌体可导致舌背麻木,若支撑架调节不当,极易出现上切牙松动、断裂现象,严重者脱落,提示评价声门区暴露情况对提高手术质量至关重要。
目前,已有许多研究针对支撑喉镜下声门区暴露困难影响因素进行分析。黎景佳等[14]研究报道,声门区暴露困难患者与性别、BMI、改良Mal-lampati分级均无关,本研究单因素分析结果与其一致;但该研究结果发现声门区暴露困难与颈围无关,与本研究结果不同,考虑可能与所选样本肥胖者较多有关。关于头颈部解剖相关指标,本研究主要测量SMD、TMA、张口度、颈部屈伸度、HMD、TMD、VTMD、HTMD的数值,结果发现SMD与术中声门区暴露困难无关,TMA、张口度、颈部屈伸度、HMD、TMD、VTMD、HTMD均与术中声门区暴露困难有关,与金晓锋等[15]研究结果基本一致,提示测量头颈部解剖相关指标有利于评估术中声门暴露困难情况。此外,除本身影响因素外,术中声门暴露困难程度还可能与支撑喉镜形状、大小及全麻下肌肉松弛程度有关,因此本文所有受试者均采用同一型号、同一麻醉方案进行研究,以尽可能避免其对研究结果的影响。
支撑喉镜手术与声门暴露相关的重要骨性结构为上下颌骨及甲状软骨,因此TMA、TMD在评估声门暴露程度上具有重要意义。金晓锋等[15]研究发现,TMA≤130°被预测为声门区暴露困难,预测灵敏度为85.7%,特异度为66.5%。秦海燕[16]研究报道,颈部自然位下的TMD、SMD与声门暴露困难有关,且TMD是声门暴露困难的独立危险因素。此外,Türkay M等[17]研究发现,颈部屈伸度<90°患者术中声门区暴露较困难,提示测量颈部屈伸度对评估声门暴露情况具有较高价值。本研究logistics多因素分析结果发现,TMA、颈部屈伸度与TMD均是影响术中声门区暴露困难的独立危险因素,与金晓锋等[15]、秦海燕[16]、Türkay M等[17]研究结果类似,提示TMA、颈部屈伸度与TMD值越小,患者术中越容易出现声门区暴露困难。
综上所述,影响支撑喉镜下声门暴露程度因素较多,尤其TMA、颈部屈伸度与TMD值对预测声门区暴露情况具有重要意义,在术前制定对应解决措施,以减少术后并发症发生。由于本研究所选样本量有限,有些影响因素未纳入,下一步应增加样本量继续研究。
[1] Roth D,Pace NL,Lee A,et al.Airway physical examination tests for detection of difficult airway management in apparently normal adult patients[J].Cochrane Database Syst Rev,2018,5:CD008874
[2] Wajekar AS,Chellaml S,Toal PV.Prediction of ease of laryn-goscopy and intubation-role of upper lip bite test,modified mal-lampati classification,and thyromental distance in various com-bination[J].J Family Med Prim Care,2015,4(1):101-105.
[3] Pinar E,Calli C,Oncel S,et al.Preoperative clinical predic-tion of difficult laryngeal exposure in suspension laryngoscopy[J].Eur Arch Otorhinolaryngol,2009,266(5):699-703.
[4] Hsiung MW,Pai L,Kang BH,et a1.Clinical predictors of diffi-cult laryngeal exposure[J].Laryngoscope,2004,114(2):358-363.
[5] Wilson ME,Spiegelhalter D,Robertson JA,et al.Predicting difficult intubation[J].Br Janaesth,1988,61(2):211-216.
[6] Cormack RS,Lehane J.Difficult tracheal intubation in obstet-rics[J].Anaesthesia,1984,39(11):1105-1111.
[7] 王敏,肖志容,余杰情,等.全麻支撑喉镜下声门暴露困难的相关因素[J].中国医学创新,2012,9(9):1-2.
[8] 薛海翔,卞文超,李海峰,等.喉癌患者行支撑喉镜下二氧化碳激光切除术后的嗓音分析及声带新生观察[J].东南大学学报(医学版),2016,35(6):979-985.
[9] Manica D,Schweiger C,Sekine L,et al.Severity of clinical manifestations and laryngeal exposure difficulty predicted by glossoptosis endoscopic grades in Robin sequence patients[J].Int J Pediatr Otorhinolaryngol,2016,90(1):270-275.
[10] 杨琛.支撑喉镜下二氧化碳激光切除术治疗声带息肉的疗效评估[J].中国内镜杂志,2016,22(7):18-21.
[11] 秦茂林,刘业海,吴开乐,等.可调式支撑喉镜下声门暴露困难患者的喉显微外科手术[J].听力学及言语疾病杂志,2016,24(2):135-138.
[12] Dion GR,Fritz MA,Teng SE,et al.Impact of vocal fold aug-mentation and laryngoplasty on dyspnea in patients with glottal incompetence[J].Laryngoscope,2017,128(2):427-429.
[13] Paul RR,Varghese AM,Mathew J,et al.Difficult Laryngeal Exposure in Microlaryngoscopy:Can it be Predicted Preopera-tively[J]?Indian J Otolaryngol Head Neck Surg,2016,68(1):65-70.
[14] 黎景佳,陈伟雄,朱肇峰,等.支撑喉镜显微手术声门区暴露困难相关因素的前瞻性研究[J].临床耳鼻咽喉头颈外科杂志,2017,31(7):33-36.
[15] 金晓锋,范国康.支撑喉镜声门暴露困难相关多因素分析[J].北京医学,2016,38(2):129-132.
[16] 秦海燕.支撑喉镜下声门暴露困难的影响因素分析[J].广西医学,2016,38(12):1708-1710.
[17] Türkay M,?entürk T,Arslan B Y,et al.Indirect laryngoscopic assessment for the diagnosis of difficult intubation in patients un-dergoing microlaryngeal surgery[J].Wien Med Wochenschr,2016,166(1):1-6.
Logistic Analysis of Influencing Factors of Glottic Exposure Difficulty in Support Laryngoscope
中图分类号: