

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 72-76.DOI: 10.3969/j.issn.1009-976X.2020.01.016
摘要:
寰枢椎的先天畸形、外伤、肿瘤、炎症等均容易引起上颈椎不稳,寰枢不稳容易造成脊髓受压,导致肢体麻木、乏力;严重者可导致瘫痪,呼吸功能障碍等而危及患者生命[1]。治疗寰枢不稳的方法众多,寰枢椎椎弓根钉内固定是治疗寰枢椎不稳的有效方法之一,但由于寰枢柱局部结构复杂,毗邻椎动脉、脊髓神经及丰富的静脉丛,损伤后容易危及生命,且寰枢椎椎弓根常有变异,因此上颈椎手术是脊柱骨科的难点[2,3]。如何提高置钉的准确性及安全性一直是临床医生思考的重大问题,数字骨科与导航模板技术的发展为临床提供解决方法。本文回顾分析自2015年1月至2018年7月在我院行的12例寰枢椎脱位及不稳病例,术前采用数字骨科设计与数字化打印导航模板,术中在导航模板下置钉,探讨其临床效果。
12例患者,男7例,女5例;年龄38~67岁,平均49.7岁。其中陈旧性齿状突骨折不愈合伴寰枢椎不稳5例,类风湿性关节炎伴寰枢椎脱位3例,齿状突游离小体伴寰枢不稳1例,新鲜Ⅱ型齿状突骨折伴横韧带断裂寰枢不稳3例。本组所有患者均有枕颈部疼痛,颈部活动受限,或伴有四肢感觉运动功能障碍。术前VAS评分3~7分,平均4.3分,术前JOA评分5~14分,平均8.4分。所有患者均行颈椎薄层CT(层厚1 mm)检查,颈椎MR检查,颈椎开口位,颈椎正侧位及颈椎动力位检查。所有患者术前均在Garden-Well牵引弓行颅骨牵引,并行床边侧位片提示:寰枢关节不稳脱位复位良好,且颈椎动力位片已经提示为可复型脱位。
患者取仰卧位,采用64排螺旋CT,术前对患者寰枢椎行CT薄层扫描(层厚1 mm,层间距0.5 mm),获得的CT数据以DICOM格式导入三维重建软件Mimics软件,进行三维图像重建,获得寰枢椎原始模型,生成STL格式文件。在Med CAD模块中,以3.5 mm圆柱模拟椎弓根钉设计,缓慢拖动圆柱体,分别在三维界面、轴面、矢状面观察圆柱体通过寰枢椎椎弓根相应骨性结构的位置关系,并确保圆柱体四壁不能穿破椎管及椎动脉等重要结构。此圆柱体即为置钉安全钉道,取寰椎后弓与枢椎棘突为模板辅助定位骨性标志,建立三维互补组件。使导向管通过连接杆同组件连接,使导向管、连接杆与互补组件融合为整体手术辅助模板。寰枢椎三维模型与手术辅助模板分别存储为STL格式文件,采用3D打印机打印出寰枢椎模型及椎弓根导向模板,导航模板行消毒,供手术过程中使用。
所有患者均在同一组医生完成手术。术中全麻,经鼻插管,口腔中塞一个绑带。术中采用俯卧位,置患者头与U型头垫(可透X-ray)上,呈微屈位,Garden-Well牵引弓行颅骨牵引,牵引重量约3 kg,采用头高脚底体位。术前拍寰枢椎正侧位片,确定手术切口及寰枢椎不稳是否复位。确定切口后,标记笔确定后方枕颈正中切口,切开周围组织,分离周围肌肉,小心剥离寰椎后弓,枢椎椎板,侧块及枢椎棘突,尽量剥离骨界面周围的软组织,力求获得一个干净的骨界面,以便术中可以方便地使用导航模板,剥离周围组织时注意勿伤及静脉丛及脊髓、椎动脉等主要结构。而后把消毒好的导航模板与寰枢椎后方结果进行贴合,观察其匹配准确性。而后助手放置导航模板,根据模板使用2.5 mm砖头顺导航通道转入约1 mm后,透视寰枢椎正侧位片,位置良好后,继续使用磨钻扩孔,顺导航通道继续转入置椎体寰枢椎前缘(术前测量数据)后再次透视寰枢椎正侧片后,随后拔出钻头,取下导板,探针探查钉道5壁骨性结构,攻丝后,再次探针探测钉道,确保安全后将适宜长度的螺钉缓慢拧入钉道。上好椎弓根钉后,患者额头垫高,恢复颈椎生理屈度,先旋紧枢椎螺钉螺帽,再旋紧寰椎螺钉螺帽,由于钛棒存在一定的屈度,螺钉旋紧时可看到寰椎轻度后移提拉复位。透视观察复位情况,复位不佳时可取出钛棒,继续预弯弧度,再次旋紧枢椎、寰椎螺钉螺帽,证实复位满意后去除颅骨牵引。用磨钻将寰椎后弓、枢锥椎板、枢椎棘突上缘去皮质,准备好植骨床放置取出的髂骨行植骨,充分止血,放置明胶海绵及引流管后,缝合伤口,注意头下斜肌与头后大直肌缝合固定于枢椎棘突上。术后给予抗感染治疗24~48 h,激素脱水治疗2~3天。术后引流量小于30 mL给予拔除伤口引流管,术后3天佩戴颈托下床活动。神经受损的患者术后加强功能锻炼。
记录患者术前、术后3天、1个月、术后3个月、术后6个月、末次随访时的颈部疼痛视觉模拟量表(VAS)评分,JOA评分。记录手术时间、出血量、术后引流量。术后行上颈椎CT扫描,按照Kawaguchi等提出的方法对置钉准确度进行分析:0级,螺钉完全在椎弓根内;1级,螺钉穿出椎弓根壁不超过2 mm,未出现并发症;2级,螺钉穿出椎弓根壁超过2 mm,未出现并发症;3级,出现临床并发症,如椎动脉、神经根损伤。
应用SPSS 13.0统计软件包处理数据,计量资料采用均数±标准差表示,计数资料以频数表示,组间比较采用χ2检验。采用重复测量单因素方差分析比较不同时间点VAS、JOA评分水平的变化,若Mauchly球形假设不成立(P<0.05),则采用Greenhouse-Geisser校正系数对其自由度进行校正。用校正后的系数进行结果分析;如果Mauchly球形假设成立(P>0.05),则采用未校正系数进行结果分析。本研究采用双侧检验,以P<0.05为差异有统计学意义。
12例患者顺利完成手术,手术时间约120~180 min,平均(148±35)min,术中失血约 100~300 mL,平均(208±45)mL,术后拔管时引流总量120~260 mL,平均(160±60)mL。术中两例出现局部静脉丛损伤出血,给予明胶海绵及止血粉压迫后止血;术中未见椎动脉损伤、脊髓及神经损伤、脑脊液漏等并发症。伤口均Ⅰ/甲级愈合。
所有患者均获得随访,平均(24.5±9.8)个月。术前、术后VAS评分、JOA评分见表格1。VAS评分同术前对比,术后3天无统计学意义(P>0.05),术后1个月、术后3个月、术后6个月、末次随访均有统计学意义(P<0.05),疼痛明显减轻;JOA评分同术前比较,术后3天无统计学意义(P>0.05),术后1个月、术后3个月、术后6个月、末次随访均有统计学意义(P<0.05),功能改善。重复测量方差分析结果显示,12例患者在VAS评分及JOA评分在不同时间点之间差异具有统计学意义(P<0.001)。12例患者一共植入48枚螺钉,寰椎及枢椎分别植入24枚,术后行颈椎CT,按照Kawaguchi等[4]提出的方法对置钉准确度进行分析,0级47枚,占97.9%;1级1枚,占2.1%;2、3级0枚。末次随访颈椎正侧位片提示植骨融合再次复查颈椎CT确定。典型病例的影像学资料见图1、2。
表1 术前、术后VAS与JOA评分方差分析
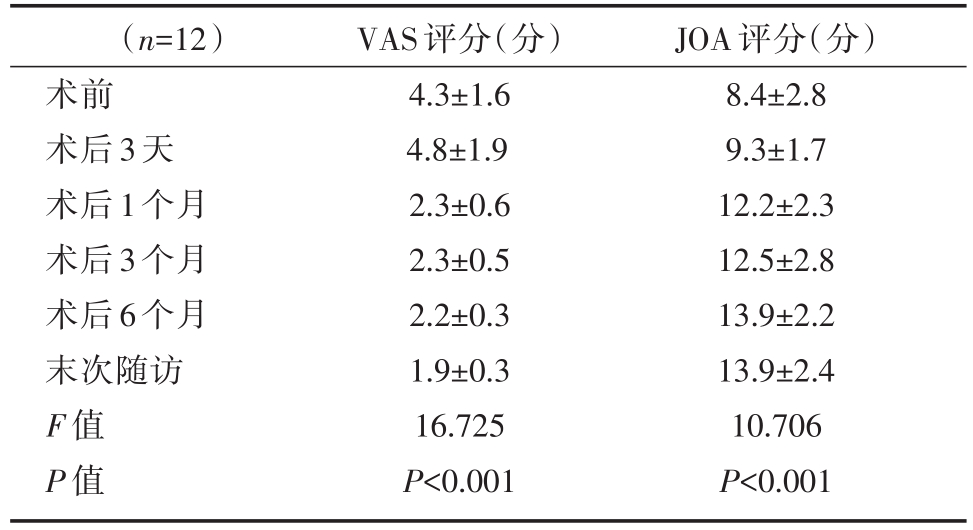
(n=12)术前术后3天术后1个月术后3个月术后6个月末次随访F值P值VAS评分(分)4.3±1.6 4.8±1.9 2.3±0.6 2.3±0.5 2.2±0.3 1.9±0.3 16.725 P<0.001 JOA评分(分)8.4±2.8 9.3±1.7 12.2±2.3 12.5±2.8 13.9±2.2 13.9±2.4 10.706 P<0.001
寰枢椎位于颅颈交界区,由于其部位深在,周围解剖结构复杂,手术难度大,风险高,一直以来是外科手术的禁区。文献报道上颈椎不稳所致寰枢椎脱位的致残率高达 60%~80%[5,6,7],严重者可能使患者瘫痪甚至危及生命,因此寰枢椎不稳传统后路钢丝及椎板夹固定技术[8],手术方法简单,但不能抗旋转,同时对于寰枢滑脱寰椎不能很好的复位;寰枢椎后路经关节螺钉固定术[9],需要在寰枢椎复位情况下行手术;前路TARP手术则多用于难复型脱位患者[10,11];而寰枢椎后路椎弓根螺钉内固定术在生物力学和临床疗效上具有明显的优越性[12]。寰枢椎后路螺钉技术实施寰枢椎脱位固定的是印度学者 Goel和德国的 Harms[13,14],因此这一技术又称为Goel-Harms技术;2002年谭明生等[15]选择寰椎后结节旁开20 mm与后弓的后下缘的交点为进钉点,内倾 10°~15°,头倾 5°~10°方向。王圣林、王超等[16]通过探测寰椎侧块的内缘进针更加简单易行。但文献报道无辅助下徒手置钉的准确率在53%~76%[17]。因此,目前经寰枢椎弓根置钉技术安全性面临的挑战是如何提高椎弓根螺钉进针点以及进钉角度的准确性,避免打爆椎弓根后出现并发症,提高手术的安全性。

图1 数字骨科导航模板
目前,数字骨科的大力发展,特别是椎弓根导航模板的发展,行寰枢椎椎弓根钉手术的安全性大大提高[11]。利用导航模板可以直观判断寰枢椎脱位类型,寰枢椎结构变异情况,有无置钉禁忌;在导航模板上可以直观的选择置钉进针点及方向,确定手术参考标记;术中还可以结合模板同手术显露局部结构对比,了解未能显露的结构,从而更加准确地操作,降低手术难度。本组的置钉准确率达97.9%,12例患者术后1个月、术后3个月、术后6个月、末次随访时的VAS评分及JOA评分均好于术前,未见术中术后并发症,虽有2例患者出现术中静脉丛出血,采用明胶海绵压迫止血。我们的经验是:①主要借助于高速螺旋CT,获取病椎的精确信息,通过电脑软件,进行病椎的重建和处理,后输入3D打印设备,打印椎弓根导航模板;②导航模板是根据椎板、棘突及关节突表面形态打印,术中需对软组织进行充分剥离,但避免损伤周围组织,使导板和相应骨性结构贴合紧密;③放置导航模板时,助手一定要稳定模板,钻孔后,反复确定进针点及方向,顺应导航模板置导针后透视,椎弓根探子探测椎弓根内外侧壁。
综上所述,术前数字骨科导航模板辅助寰枢椎椎弓根螺钉置钉是一种置钉准确性高,安全、有效、可靠的方法。作为一个高难度手术在术前数字骨科的模拟,术中导航模板的应用使得学习曲线更加短,降低手术难度。但本组资料样本少,需要多中心大样本长期随访数据进一步分析其远期疗效及并发症。
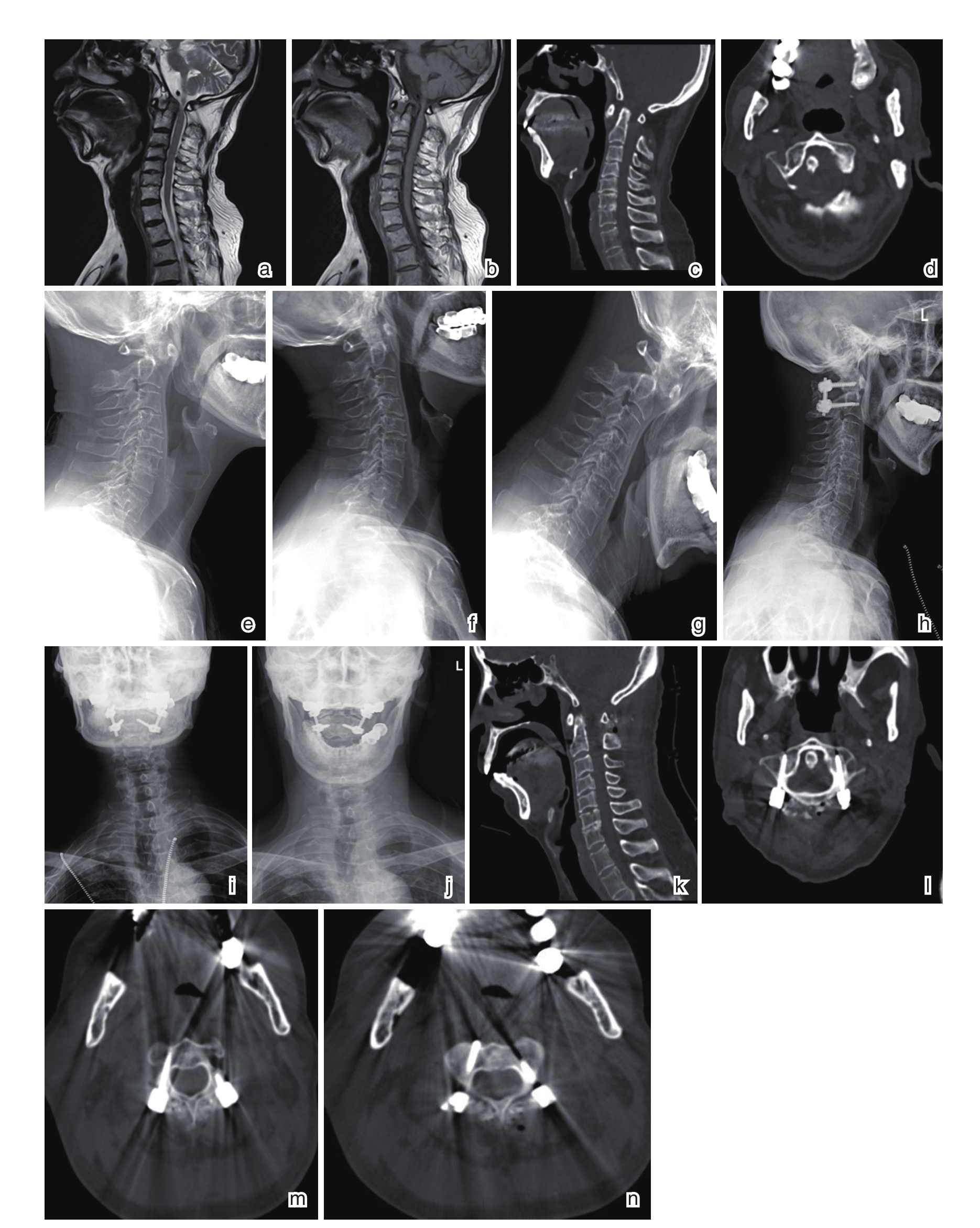
图2 患者男性,57岁,诊断为类风湿性关节炎寰枢椎不稳(可复型)
a、b:颈椎MRT2、T1像,脊髓受压;c、d:颈椎CT,寰枢关节脱位不稳;e、f、g:术前颈椎侧位、动力位片提示可复型不稳;h、i、j:术后颈椎正侧位+开口位片提示完全复位,内固定位置良好;k、l、m、n:术后颈椎CT提示:椎弓根钉位置良好
[1] 尹庆水,王建华.寰枢椎脱位的治疗进展[J].中华骨科杂志,2015,35(5):586-594.
[2] 王建华,尹庆水,夏虹,等.综合应用现代影像学技术对上颈椎骨折脱位85例诊疗分析[J].实用医学杂志,2006,22(10):1176-1177.
[3] 吴鑫杰,谭明生.寰枢椎后路内固定技术的研究进展[J].中国矫形外科杂志,2019,26(6):528-532.
[4] Kawaguchi Y,Nakano M,Yasuda T,et al.Development of a new technique for pedicle screw and Magerl screw insertion us-ing a 3-dimensional image guide[J].Spine(Phila Pa l976),2012.37(23):1983-1988.
[5] Yang SY,Boniello AJ,Poorman CE,et al.A review of the diag-nosis and treatment of atlantoaxial dislocations[J].Global Spine J,2014,4(3):197-210.
[6] Syre P,Petrov D,Malhotra NR.Management of upper cervical Spine injuries:a review[J].J Neurosurg Sci,2013,57(3):219-240.
[7] Wang F,Li CH,Liu ZB,et al.The effectiveness and safety of 3-dimensional printed composite guide plate for atlantoaxial pedicle screw:A retrospective study[J].Medicine(Balti-more),2019,98(1):e13769.
[8] Jacobson ME,Khan SN,An HS.C1-C2 posterior fixation:indi-cations,technique,and results[J].Orthop Clin North Am,2012,43(1):11-18.
[9] Elliott RE,Tanweer O,Boah A,et al.Atlantoaxial fusion with transarticular screws:meta-analysis and review of the literature[J].World Neurosurg,2013,80(5):627-641.
[10] Yin Q,Ai F,Zhang K,et al.Irreducible anterior atlantoaxial dislocation:one stage treatment with a transoral atlantoaxial re-duction plate fixation and fusion.Report of 5 cases and review of the literature[J].Spine(Phila Pa 1976),2005,30(13):E375-E381.
[11] 夏虹,王建华,吴增晖,等.3D打印技术辅助经口前路个性化手术治疗复杂颅颈交界区畸形[J].中华创伤杂志,2016,32(1):21-26.
[12] Tan M,Wang H,Wang Y,et al.Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass[J].Spine(Phila Pa 1976),2003,28(9):888-895.
[13] Goel A,Desai KI,Muzumdar DP.Atlantoaxial fixation using plate and screw method:a report of 160 treated patients[J].Neurosurgery,2002,51(6):1351-1357.
[14] Harms J,Melcher RP.Posterior C1-C2 fusion with polyaxial screw and rod fixation[J].Spine(Phila Pa 1976),2001,26(22):2467-2471.
[15] 谭明生,张光铂,李子荣,等.寰椎测量及其经后弓侧块螺钉固定通道的研究[J].中国脊柱脊髓杂志,2002,12(1):5-8.
[16] 王圣林,王超,阎明,等.寰枢侧块钉板固定术第1颈椎侧块螺钉置人准确性的分析[J].中华外科杂志,2008,46(2):115-117.
[17] Mueller CA,Roesselcr L,Podlogar M,et al.Accuracy and complications of transpedicular C2 screw placement without the use of spinal navigation[J].Eur Spine J,2010,19(5):809-814.
Clinical efficacy of digital orthopaedic technique and navigation template assisted atlantoaxial personalized pedicle screw placement
中图分类号: