

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 44-54.DOI: 10.3969/j.issn.1009-976X.2020.01.010
摘要:
过去的几十年中,基于浸润性乳腺癌的国家和国际治疗指南的不断变化,乳腺癌腋窝清扫的重新定义尤其是哨兵节点概念的实现,减少了手术激进主义,而不损害肿瘤学的安全性或诊断准确性[1-3]。保乳手术(BCS)是治疗乳腺癌的常用方法,其目的是去除所有恶性组织的同时确保良好的美容效果,其存活率与乳腺切除术相似[4,5]。但部分初次保乳手术后患者常需要再次切除[6],因此,改良的乳腺癌根治术(MRM)作为早期乳腺癌的另一个治疗方法仍适用和被广泛接受。另一方面,虽然生存率提高,但乳腺癌在生理、心理和社会方面对个体产生的影响仍存在,如这些因素对年龄较小、健康状况较差的妇女产生更多的负面影响[7]。针对患者术后面临的问题如放化疗、乳房重建、经济状况、不良反应等,不同患者存在着差异。本研究旨在探讨乳腺癌改良根治术(MRM)保乳手术(BCS)患者在选择手术方式的差异并作分析。
采用前瞻性研究方法,时间为2016年10月~2018年12月就诊于本院并接受相应治疗的早期乳腺癌患者作为研究对象,纳入标准为符合早期乳腺癌临床相关诊断标准且符合相应手术指征者。排除标准:①存在精神障碍或心理障碍者;②患有严重传染性疾病或重大心血管疾病者;③不符合本次研究其他相关标准者。最终获得完整资料的入组患者共72例,包括接受保乳手术患者36例(保乳组),接受改良根治手术患者36例(改良根治组)。
所有患者均接受严格的术前谈话,具体内容包括:①流行病学情况;②手术方式、方法、切除范围和淋巴结清扫情况;③术后放疗、化疗、系统治疗(包括内分泌治疗)的过程、时间;④各阶段费用;⑤并发症、不良反应以及复发情况。最终由患者选择术式。所有患者在出院后接受6月随访,包括临床表现、并发症、不良反应、身体意象、生活质量的数据收集。
1.2.1 乳腺癌改良根治术组 患者取平卧患肢外展位,麻醉成功后常规消毒铺巾,取包括乳头乳晕,乳腺肿物在内的梭形手术切口,切开皮肤及皮下组织,分离皮瓣上至锁骨下,下至腹直肌前鞘,内至胸骨旁,外至背阔肌前缘,沿胸大肌表面将乳房切除,并沿胸大肌外缘暴露左侧腋静脉,打开腋静脉鞘,暴露胸长神经,胸背神经及其伴行血管,切除左腋窝组织,创面彻底止血,予温灭菌注射用水冲洗创面,在胸壁及腋窝各留置一条引流管,予固定,用丝线间断缝合手术切口,术后加压包扎。
1.2.2 保乳组 取平卧患肢外展位,麻醉成功后常规消毒铺巾,沿原手术切口取梭形切口,切开皮肤及皮下组织,切除原肿瘤周围约2 cm腺体组织,于残腔周围腺体取7个点组织送冰冻未见癌浸润,温灭菌注射用水冲洗创面,于瘤床位置放置4枚钛夹标记,用可吸收线间断缝合手术切口。再沿胸大肌外缘暴露腋静脉,打开腋静脉鞘,暴露胸长神经,胸背神经及其伴行血管,切除腋窝组织,创面彻底止血,予温灭菌注射用水冲洗创面,在腋窝留置一条引流管,予固定,用丝线间断缝合手术切口,术后加压包扎。
①由参与本次研究的临床观察小组收集手术相关指标(手术耗时、术中出血量、引流量、住院耗时)、切除乳腺重量;②术后并发症发生情况(皮下组织积液、切口感染、皮肤萎缩、淋巴性水肿);③影响患者手术选择的因素;④生活质量(生理机能、精神状态、社会功能、物质生活)进行观察记录和对比分析,并同时客观评估其乳房美观效果(优:患者术后乳房几乎完全对称,且两侧乳头水平差距≦2 cm;良:患者术后乳房基本较对称,且两侧乳头水平差距≦3 cm;差:患者术后乳房明显不对称,且两侧乳头水平差距>3 cm)。
采用体像量表(BIS)对身体意象进行评价。十项量表包括情感项目、行为项目和认知项目,总分从0到30不等。分数越高表示身体形象越差[8]。
患者于手术后6月完成生活质量调查表(QLQ-C30 和 QLQ-BR23)的功能量表[9],包括情绪、身体、角色、社交和认知功能以及总生活质量。同时,三个多项目量表和五个单项目子量表评估症状采用例数表示,如食欲减退、便秘、腹泻、失眠和呼吸困难,全身治疗副作用、手臂症状、乳腺症状、身体意象和性功能。
将本研究所有相关数据进行初步筛选与整理后逐一录入至SPSS 20.0统计学软件中进行科学性分析,计量资料以均数±标准差表示,运用t检验,对计数资料则通过卡方检验进行比较,P<0.05为数据存在统计学差异。
比较保乳组患者与改良根治组患者的年龄、肿瘤部位、肿瘤分期、淋巴转移、形态、分化程度、放疗等一般资料,差异无统计学意义(P>0.05),详见表1。
表1 两组患者基本临床特征[n(%)]

保乳组(n=36)改良根治组(n=36) 统计值P值年龄/岁多灶性/例肿瘤部位/例外象限内象限乳晕部内外象限交界肿瘤分期/例T1a T1b T1c T2淋巴结转移/例N0 N1 N2形态学/例导管型小叶型分化程度/例高分化中分化高分化激素受体状况/例阴性阳性HER2/例阴性阳性腋窝淋巴结清扫/例32.86±5.94 16(44.44)33.41±4.27 14(38.89)-0.450 0.534 1.471 0.654 0.465 0.689 10(27.78)7(19.44)8(22.22)11(30.56)12(33.33)10(27.78)6(16.67)8(22.22)0.4030.940 6(16.67)13(36.11)10(27.78)7(19.44)8(22.22)12(33.33)10(27.78)6(16.67)0.2710.873 18(50.00)12(33.33)6(16.67)16(44.44)14(38.89)6(16.67)0.2230.637 20(55.56)16(44.44)18(50.00)18(50.00)0.3550.837 16(44.44)14(38.89)6(16.67)15(41.67)13(36.11)8(22.22)0.2250.635 19(52.78)17(47.22)21(58.33)15(41.67)0.2290.633 16(44.44)20(55.56)14(38.89)22(61.11)0.6050.437有无24(66.67)12(33.33)27(75.00)9(25.00)放疗/例0.5000.479有无17(47.22)19(52.78)20(55.56)16(44.44)系统治疗/例N0内分泌治疗化疗内分泌+化疗1.1910.755 10(27.78)8(22.22)10(27.78)8(22.22)9(25.00)12(33.33)9(25.00)6(16.67)
比较保乳组与根治组患者手术时间、手术出血量、引流量、住院耗时、切除组织重量、乳房美观性,差异具有统计学意义(P<0.05),详见表2。
两组经济条件、复发恐惧、形象影响、生育愿望相比存在统计学意义(P<0.05),可见经济条件、复发恐惧、形象影响、生育愿望是影响患者手术选择的主要因素,详见表3。
两组患者的功能量表评分相比无差异(P>0.05),在比较两组疲劳、呕吐、疼痛、失眠、财政困难、乳房症状、脱发症状发生率,差异具有统计学意义(P<0.05)。
早期乳腺癌属于乳腺癌的早期阶段且永久性治愈的概率相对较高。改良根治术是目前治疗早期乳腺癌的常见措施,尽管其能够在一定程度上尽可能地确保患者胸小肌等部位的完好性,但其所需切除范围较广,术后易影响患者的形体美观效果,不仅不利于术后病情的良好发展,同时还易对其生活质量带来负面影响。保乳术出血量低、手术耗时短,术后乳房及形体完好性与对称性维持了形体的美观性,使保乳手术总体生活质量高于乳癌根治术。
早期的临床研究表明,单独BCS或乳腺切除术治疗的早期浸润性乳腺癌,其长期生存率相当[4]。早期研究已证实BCS加放疗可减少局部复发,提高生存率[10],目前保乳手术包括肿瘤切除术后放射治疗,其效果至少等同于甚至优于乳腺切除术[11],这表明根治性手术可能不会为乳腺癌患者的总体生存率提供额外的好处。乳房切除术更常用于晚期乳腺癌的女性。
与乳房切除术患者相比,BCT组患者表现出更好的情感、社交和角色功能。先前的研究也报道了实施保乳的乳腺癌患者与乳房切除术比较时,在生活质量等方面显示出的优势[12-14]。甚至复发性乳腺癌患者保乳术后生活质量分数高于健康女性人群样本[15]。Schou等研究报告显示,乳腺癌患者的总体生活质量得分高于健康女性[16]。与没有癌症经历的普通人群相比,乳腺癌患者的总体生活质量得分更高的原因可以用“重新定义”的概念来解释。但是,作者认为乳房切除术可能减少乳腺癌患者对肿瘤发展的恐惧,可能患者考虑的是肿瘤切除的更广泛(表3)。
表2 两组手术相关指标
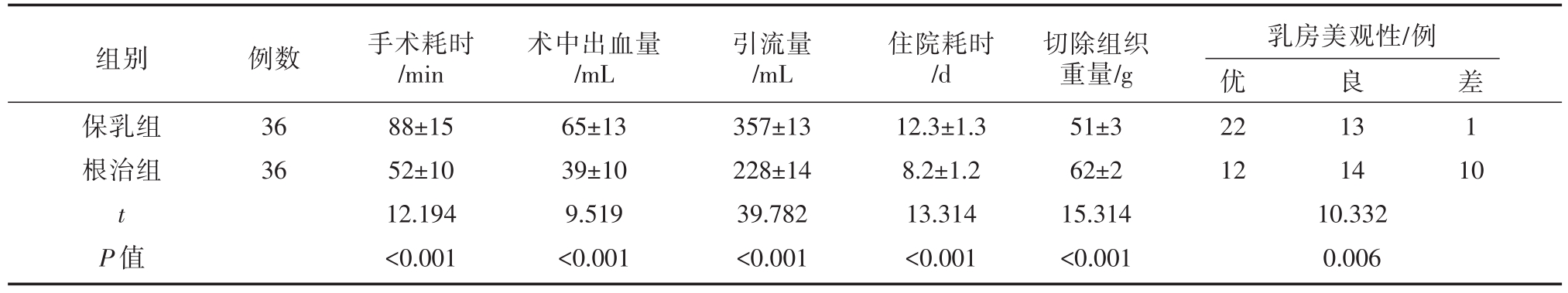
组别保乳组根治组t P值例数36 36手术耗时/min 88±15 52±10 12.194<0.001术中出血量/mL 65±13 39±10 9.519<0.001引流量/mL 357±13 228±14 39.782<0.001住院耗时/d 12.3±1.3 8.2±1.2 13.314<0.001切除组织重量/g 51±3 62±2 15.314<0.001乳房美观性/例优22 12 10.332 0.006良13 14差1 1 0
表3 影响患者手术选择的因素

年龄/岁文化程度/例大学以上大学高中初中及以下经济条件/例高收入中收入低收入身体形象影响/例放化疗恐惧/例复发恐惧/例婚姻状态/例已婚未婚离婚生育愿望/例保乳组32.86±5.94改良根治组33.41±4.27统计值-0.450 1.286 P值0.654 0.732 6(16.67)15(41.67)8(22.22)7(19.44)10(27.78)13(36.11)7(19.44)6(16.67)19.238<0.001 15(41.67)16(44.44)5(13.89)30(83.33)30(83.33)31(86.11)5(13.89)8(22.22)23(63.89)15(41.67)32(88.89)16(44.44)13.333 0.465 13.787 1.188<0.001 0.496<0.001 0.552 17(47.22)9(25.00)10(27.78)20(55.56)6(16.67)10(27.78)23.063<0.001有无15(41.67)21(58.33)34(94.44)2(5.56)
表4 乳腺癌患者的生活质量(QLQ-C30和-BR23量表)
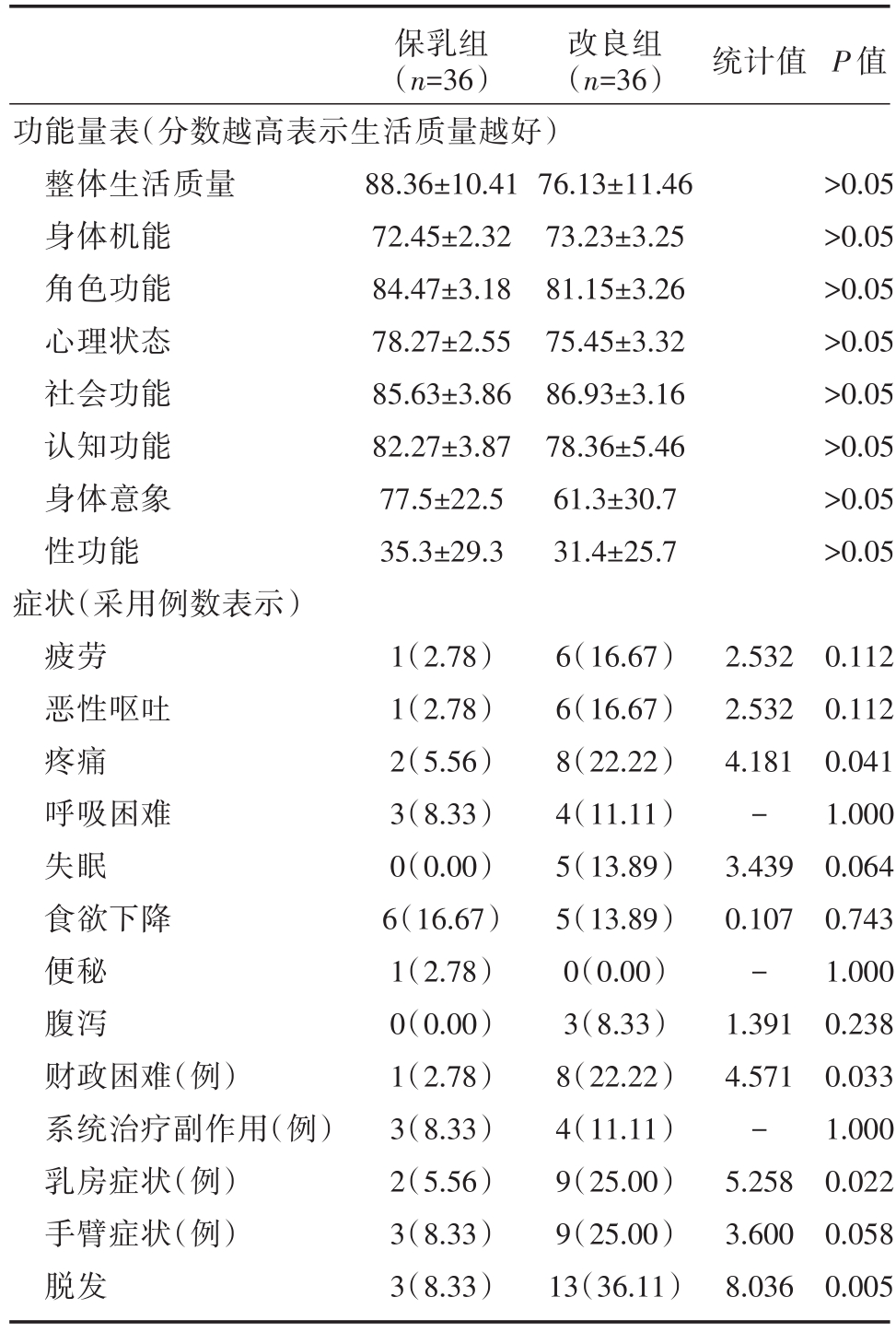
注:功能量表(分数越高表示生活质量越好);症状量表(分数越低表示生活质量越好)
保乳组(n=36)改良组(n=36) 统计值P值功能量表(分数越高表示生活质量越好)整体生活质量身体机能角色功能心理状态社会功能认知功能身体意象性功能症状(采用例数表示)疲劳恶性呕吐疼痛呼吸困难失眠食欲下降便秘腹泻财政困难(例)系统治疗副作用(例)乳房症状(例)手臂症状(例)脱发88.36±10.41 72.45±2.32 84.47±3.18 78.27±2.55 85.63±3.86 82.27±3.87 77.5±22.5 35.3±29.3 76.13±11.46 73.23±3.25 81.15±3.26 75.45±3.32 86.93±3.16 78.36±5.46 61.3±30.7 31.4±25.7>0.05>0.05>0.05>0.05>0.05>0.05>0.05>0.05 1(2.78)1(2.78)2(5.56)3(8.33)0(0.00)6(16.67)1(2.78)0(0.00)1(2.78)3(8.33)2(5.56)3(8.33)3(8.33)6(16.67)6(16.67)8(22.22)4(11.11)5(13.89)5(13.89)0(0.00)3(8.33)8(22.22)4(11.11)9(25.00)9(25.00)13(36.11)2.532 2.532 4.181-3.439 0.107-1.391 4.571-5.258 3.600 8.036 0.112 0.112 0.041 1.000 0.064 0.743 1.000 0.238 0.033 1.000 0.022 0.058 0.005
本研究的一个重要的缺陷是缺乏患者术前的基线生活质量数据,因此无法分析手术治疗前后生活质量的变化。另外,作者在完成问卷调查过程中同质性不够,以及部分患者并不积极参与调查,结果不一定完全具有代表性。总之,我们的研究结果进一步显示出保乳手术在治疗早期乳腺癌的手术选择方面具有优势,这符合以往的研究报告。
[1] Veronesi U,Paganelli G,Viale G,et al.A randomized compari-son of sentinel-node biopsy with routine axillary dissection in breast cancer[J].N Engl J Med,2003,349(6):546-553.
[2] Bergkvist L,de Boniface J,Jönsson PE,et al.Axillary recur-rence rate after negative sentinel node biopsy in breast cancer:three-year follow-up of the Swedish Multicenter Cohort Study[J].Ann Surg,2008,247(1):150-156.
[3] Warrier S,Tapia G,Goltsman D,Beith J.An update in breast cancerscreeningand management [J].WomensHealth(Lond),2016,12(2):229-239
[4] Fisher B,Anderson S,Bryant J,et al.Twenty-year follow-up of a randomized trial comparing total mastectomy,lumpectomy,and lumpectomy plus irradiation for the treatment of invasive breast cancer[J].N Engl J Med,2002,347(16):1233-1241.
[5] Winchester DJ,Menck HR,Winchester DP.The National Can-cer Data Base report on the results of a large nonrandomized comparison of breast preservation and modified radical mastecto-my[J].Cancer,1997,80(1):162-167.
[6] Talsma AK,Reedijk AM,Damhuis RA,et al.Re-resection rates after breast-conserving surgery as a performance indicator:introduction of a case-mix model to allow comparison between Dutch hospitals[J].Eur J Surg Oncol,2011,37(4):357-363
[7] Ohsumi S,Shimozuma K,Kuroi K,et al.Quality of life of breast cancer patients and types of surgery for breast cancer—current status and unresolved issues[J].Breast Cancer,2007,14(1):66-73.
[8] Hopwood P,Fletcher I,Lee A.A body image scale for use with cancer patients[J].Eur J Cancer,2001,37(2):189-197.
[9] Tan ML,Idris DB,Teo LW,et al.Validation of EORTC QLQ-C30 and QLQ-BR23 questionnaires in the measurement of quali-ty of life of breast cancer patients in Singapore[J].Asia Pac J Oncol Nurs,2014,1(1):22-32.
[10] Veronesi U,Luini A,Del Vecchio M,et al.Radiotherapy after breast-preserving surgery in women with localized cancer of the breast[J].N Engl J Med,1993,328(22):1587-1591.
[11] Arriagada R,Lê MG,Rochard F,Contesso G.Conservative treatment versus mastectomy in early breast cancer:patterns of failure with 15 years of follow-up data.Institut Gustave-Roussy Breast Cancer Group[J].J Clin Oncol,1996,14(5):1558-1564.
[12] Chow R,Pulenzas N,Zhang L.Quality of life and symptom bur-den in patients with breast cancer treated with mastectomy and lumpectomy[J].Support Care Cancer,2016,24(5):2191 -2199.
[13] Engel J,Kerr J,Schlesinger-Raab A.Quality of life following breast-conserving therapy or mastectomy:results of a 5-year pro-spective study[J].Breast J,2004,10:223-231.
[14] He Z-Y,Tong Q,Wu S-G.A comparison of quality of life and satisfaction of women with early-stage breast cancer treated with breast conserving therapy versus mastectomy in southern China[J].Support Care Cancer,2012,20(10):2441-2449.
[15] Jendrian S,Steffens K,Schmalfeldt B,et al.Quality of life in patients with recurrent breast cancer after second breast-conserv-ing therapy in comparison with mastectomy:the German experi-ence[J].Breast Cancer Res Treat,2017,163(3):517-526.
[16] Schou I,Ekeberg O,Sandvik L.Multiple predictors of health-related quality of life in early stage breast cancer.Data from a year follow-up study compared with the general population[J].Qual Life Res,2005,14(8):1813-1823.
Comparison of breast conserving operation and modified radical operation in the treatment of early breast cancer
中图分类号: