

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 25-28.DOI: 10.3969/j.issn.1009-976X.2020.01.006
摘要:
目前常规腹腔镜胆囊切除术(LC)多采用标准的三孔或四孔法,分别为脐下缘(10 mm),剑突下(10 mm),右锁中线肋缘下(5 mm),有或无右腋前线肋缘下(5 mm),标准的腹腔镜胆囊切除后从剑突下戳卡口取出标本,对于胆囊结石较大,胆囊壁增厚明显等病例常较困难,往往需要延长剑突下切口。目前临床上有商用的标本取出器使用较方便,但价格较贵;我们利用一次性无菌乳胶手套自制带延长荷包线的改良标本取出袋,缩小剑突下戳卡口,以减轻腹直肌损伤,从脐部戳卡口取出胆囊标本,临床效果较明显,现报道如下。
本次研究纳入南通市第六人民医院普外科2018年1月至2018年12月接受择期腹腔镜胆囊切除术的胆囊良性疾病患者(纳入标准:经B超与核磁诊断为胆囊结石合并胆囊炎患者;排除标准:①合并胆管结石及腹膜炎者;②有上腹部手术史者;③有出血倾向者(INR>1.5,血小板<100×109/L);④过度肥胖患者(BMI> 28 kg/m2);⑤术前高度怀疑胆囊恶性疾患者;⑥不能耐受气腹和全麻者及ASA评分>III级者。按入院次序单双数分为两组,分别为利用自制带延长荷包线改良标本取出袋自脐部切口取出胆囊(改良组)及常规于剑突下切口取出胆囊(常规组),最后58例患者入组,包括改良组30例,常规组28例。两组患者手术均由同一主刀医生完成,术后均使用配方一致的镇痛泵镇痛,常规吸氧,心电血氧监测6小时,麻醉完全清醒后可下床活动,术后定期检创,观察切口愈合情况;术后常规使用抗生素,进半流质食后无不适症状容许出院,因患者随访时间短,故未将戳卡口疝发生率作为主要评价指标。
将一次性无菌手套在靠近手指分岔处剪去多余手指套,近断端用普通4号丝线双重结扎,手套口处用两根4号或7号丝线连接后做荷包缝合,以便于装取胆囊,见图1。

图1 腹腔镜手术中自制改良标本袋 a标本袋荷包开放状态;b标本袋荷包收紧状态
LC手术均采用全麻、CO2建立气腹,常规取腹壁脐下方观察孔(A孔10 mm)、剑突下操作孔(B孔5 mm或10 mm)、右锁中线肋缘下操作孔(C孔5 mm),常规组B孔10 mm,改良组B孔5mm,两组均顺利切除胆囊,检查无渗血及胆漏后,常规组由B孔用自制改良标本袋取出胆囊标本,改良组将自制改良标本袋由A孔置入腹腔,线尾置于体外,装取胆囊后经A孔取出胆囊标本,手术步骤见图2(a-f)。常规组用4号可吸收缝线分层缝合剑突下及脐部10 mm戳卡口,改良组只缝合脐部10 mm戳卡口。
开腹中转率及术中,术后并发症:术中并发症定义为从麻醉开始至返回病房期间的并发症;术后并发症定义为术后1周内发生的与手术相关的并发症。手术时间:手术时间定义为从切皮至缝合完皮肤的时间;术后疼痛缓解时间:术后疼痛缓解时间定义为患者全麻术后清醒后至疼痛评分降至NRS评分三分以下的时间;术后住院时间:患者术后血常规,肝功无明显异常,胃肠道功能完全恢复,进食半流食后无明显不适感后允许出院;术后住院时间以患者术后住院的夜间计算;术中费用和总费用:包括患者麻醉,手术及术中使用器械及耗材的费用总和。
术后疼痛程度评分:术后自觉疼痛程度采用NRS评分量表,患者被要求用数字(0~10)表达出感受疼痛的强度,0分没有疼痛,1~3分轻度疼痛,4~6分中度疼痛,7~10分重度疼痛,分值越高,表示疼痛程度越重。
采用统计学软件SPSS 24.0进行统计学分析,正态分布计量资料比较采用均数±标准差表示,采用独立t检验;计数资料组间比较χ2检验,P<0.05表示差异有统计学意义。
两组患者入院时在性别、年龄、手术适应症、体重指数及术前麻醉评分上的差异无统计学意义,基线一致,具有可比性。表1。
两组患者在中转开腹例数、术中术后并发症发生率、手术时间以及治疗费用上无统计学意义(P>0.05);改良组在术后疼痛持续时间及术后6、12、24、36小时疼痛程度评分上显著优于常规组(P<0.05);见表2、表3。
表1 两组患者一般情况比较
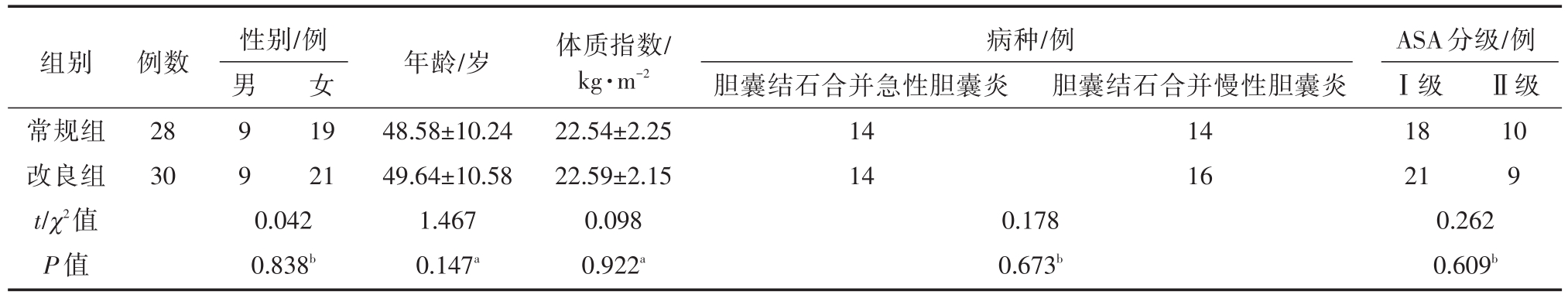
注:at检验;bX2检验
性别/例组别常规组改良组t/χ2值P值例数28 30男9 9女19 21胆囊结石合并慢性胆囊炎14 16Ⅱ级10 9 0.042 0.838b年龄/岁48.58±10.24 49.64±10.58 1.467 0.147a体质指数/kg·m-2 22.54±2.25 22.59±2.15 0.098 0.922a病种/例胆囊结石合并急性胆囊炎14 14 0.178 0.673b ASA分级/例Ⅰ级18 21 0.262 0.609b
表2 两组患者手术后临床指标

注:*P<0.05,与常规组比较,差异有统计学意义。
组别常规组改良组t/X2值P值中转开腹/例 术中术后并发症/例胆漏 胆道损伤 切口周围血肿 切口脂肪液化及感染0 0 0 0 0 0 1 0 0 0 3.0 0.223手术时间/min 42.38±7.25 45.85±6.25 0.372 0.640术后疼痛持续时间/h 52.38±7.25 32.85±6.25 2.232 0.010*
表3 术后临床资料

组别常规组改良组t/X2值P值术后疼痛程度评分(NRS)术后6小时5.8±0.75 4.5±0.85 2.596 0.010术后12小时5.9±0.85 4.4±0.75 2.178 0.028术后24小时4.1±0.95 2.9±0.45 2.227 0.016术后36小时2.05±0.38 1.2±0.35-4.576 0.001术后住院时间/d 3.9±0.75 3.8±0.69 1.898 0.062治疗费用/元12950.7±954.75 12800.5±885.75 0.225 0.320
腹腔镜胆囊切除术已经为胆囊良性疾病治疗的金标准[1],随着腹腔镜技术的大量开展和手术相关器械的不断改进,双孔及单孔以及经自然腔道的腹腔镜胆囊切除技术,尤其是经脐部单孔腹腔镜胆囊切除术是近几年人们关注的焦点,其微创理念优于传统腹腔镜手术[3]。但有研究表明单孔的学习曲线比多孔腹腔镜更长[4],适应症主要局限于BMI≤30 kg/m2的单纯性疾病患者,而且术前选择发生中转手术的可能性低的患者[5]。
现代外科医生不单只注重手术的临床结果,对手术给患者所带来的术后切口疤痕的美观和创伤也越来越重视,近几年提出的快速康复理念是现代外科手术的一种趋势,也更加符合患者心理和生理的需求。以前标准的三孔或四孔法是将胆囊从剑突下10 mm戳卡孔处直接取出,有较多弊端:如胆囊壁较薄,用力提出胆囊时容易破裂,胆汁污染切口及腹腔,或结石遗留于戳卡口处或掉入腹腔,出现切口感染,有研究表明腹腔镜胆囊切除术后感染的发生率为2%~13.8%,其中切口感染约占75%[6],LC后主要以剑突下戳卡口疼痛为主[7],而经剑突下戳卡口取胆囊标本,术后疼痛持续时间及疼痛强度增加。随着专用胆囊标本取出器的出现,较好地解决了术后腹腔污染及切口感染的问题,但对剑突下戳卡口疼痛的问题仍无法有效解决,而且因专用胆囊取出器费用昂贵,且医保无法报销,增加了患者经济负担,在某种程度上也限制了其在基层医院的临床使用,因此我们借鉴专用胆囊取出器的特点,在临床上将一次性无菌手套经过改良制成取物袋,安全性好,可靠性高,而且非常便宜,取得了较好的临床效果,但也有部分胆囊过大或胆囊壁较厚,胆囊内结石较多患者在胆囊取出过程中存在取出困难,取物袋破裂风险,目前还没有合适的腔镜下经脐孔取胆囊的商用取物袋上市,我们正在考虑用其它商用取物袋改良并准备申请专利,以避免或减少这种风险。
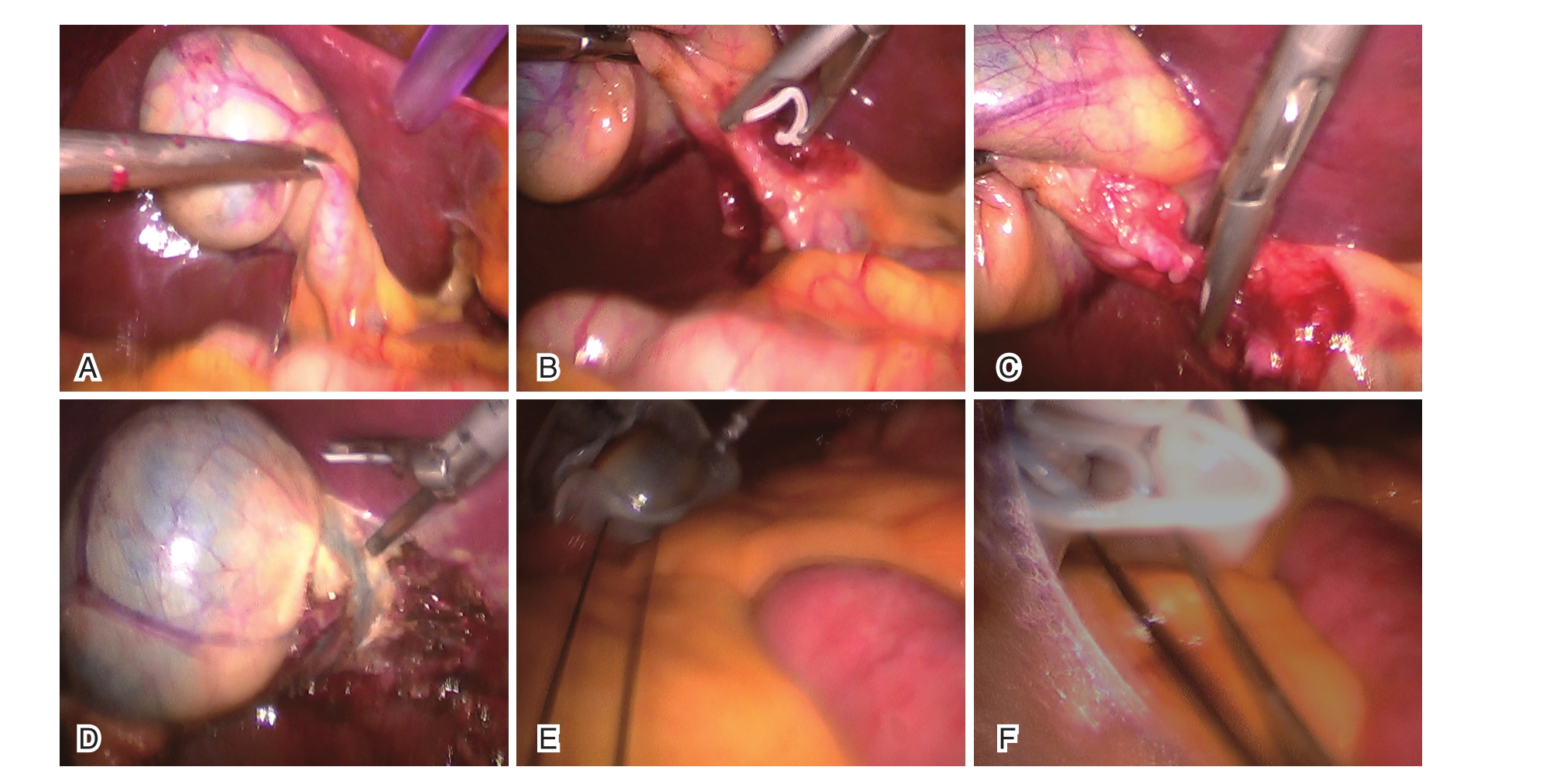
图2 手术步骤
A.显露胆囊三角;B.5 mm Hem-o-lok夹夹闭胆囊管;C.5 mm Hem-o-lok夹夹闭胆囊动脉;D.游离胆囊;E.用自制标本袋取出胆囊;F.经脐部戳卡孔取出胆囊
本研究中所有患者都严格控制手术适应症,LC手术均获成功,常规组与改良组平均手术时间及术后住院时间相近,无明显差异;无中转开腹患者,术中及术后并发症也无明显差异(P>0.05),但在手术操作过程中改良组中有一例患者在从脐孔牵拉出胆囊时荷包线断裂致取物袋脱落入腹腔,重新进镜辅助由脐孔处取出,手术时间略长,考虑是因为经脐取出标本袋时无腔镜监视,影响了操作的精确性,如使用特制专用标本取出袋可望克服此不足之处。本次研究显示在术后改良组患者疼痛持续时间均较常规组缩短(P<0.05),疼痛程度明显下降(P<0.01),可在一定程度上说明改良组较常规组对患者的创伤更小,应激反应更轻;两组患者总住院费用无明显差异,但在术中费用上改良组较常规组中使用商用取物器患者费用降低;术后住院时间改良组较常规组无明显差异,平均术后住院时间3~5天左右,与Oscar Vidal等[8]报道的术后进食时间<6小时,术后住院时间<24小时有一定差异,考虑与医院的床位使用率及不同种族的人口体质、生活习惯有关。近年来随着腹腔镜手术普及,腔镜术后戳孔疝发生率有所升高,国外报道其发生率约 0.14%~22%[9],有研究[10]表明戳孔疝的发生与戳卡直径、部位、患者年龄、是否肥胖、组织是否分层对合、感染、术后腹内压剧增等因素有关。国外有学者认为对于腹部10 mm及以上戳卡孔应仔细缝合筋膜层,以预防戳孔疝的发生[11],而肥胖患者发生戳孔疝机率更大,本研究中两组患者术后随访时间较短,在术后切口疝发生率上未做统计,也是本次研究不足之处。
总之,对于胆囊良性疾病LC术后经脐部还是在剑突下戳卡口取出胆囊标本在手术过程、手术并发症及愈后无明显差异[12,13],但经脐部取胆囊标本患者术后疼痛持续时间短,疼痛强度更轻,术后剑突下切口免缝合、遗留癖痕较小、更加美观、剑突下戳孔疝发生率低,又可以为患者节省部分医疗费用。
[1] Shaikh HR,Abbas A,Aleem S,Lakhani MR.Is mini-laparo-scopic cholecystectomy any better than the gold standard?A comparative study[J].J Minim Access Surg,2017,13(1):42-46.
[2] Mintz Y,Horgan S,Cullen J,et al.NOTES:a review of the technical problems encountered and their solutions[J].J Lapa-roendosc Adv Surg Tech A,2008,18(4):583-587.
[3] 中华医学会外科学分会胆道外科学组.胆囊良性疾病治疗决策的专家共识(2011版)[J].中华消化外科杂志,2011,10(1):14-19.
[4] Sandberg EM,la Chapelle CF,van den Tweel MM,et al.Lapa-roendoscopic single-site surgery versus conventional laparosco-py for hysterectomy:a systematic review and meta-analysis[J].Arch Uynecol Obstet,2017,295(5):1089-1103.
[5] Lirici MM,Tierno SM,Ponzano C.Single-incision laparoscopic cholecystectomy:does it work? A systematic review[J].Surg Endosc,2016,30(10):4389-4399.
[6] 刘全民.腹腔镜胆囊切除术术后特殊并发症分析[J].中华腔镜外科杂志(电子版),2011,4(2):66-67.
[7] 吴进,汪正平,颜涛,等.布比卡因切口局部浸润对腹腔镜胆囊切除术后切口疼痛的影响[J].临床麻醉学杂志,2010,26(1):30-32.
[8] Vidal O,Valentini M,Espert JJ,et al.Laparoendoscopic single-site cholecystectomy:a safe and reproducible alternative[J].Laparoendosc Adv Surg Tech A,2009,19(5):599-602.
[9] Hussain A,Mahmood H,Singhal T,et al.Long-term study of port-site incisional hernia after laparoscopic procedures[J].JSLS,2009,13(3):346-349.
[10] 李钟声,程卫,孙弢,等.腹腔镜戳孔并发症再次手术处理4例报告[J].腹腔镜外科杂志,2016,21(7):510-513.
[11] Yamamoto M,Minikel L,Zaritsky E.Laparoscopic 5 mm trocar site herniation and literature review[J].JSLS,2011,15(1):122-126.
[12] 陈小伍,王卫东,陈坚平,等.经脐单孔腹腔镜胆囊切除术与传统腹腔镜胆囊切除术的比较[J].岭南现代临床外科,2014,14(1):41-43.
[12] 杨刚,冷政伟,李勇,等.改良三孔法与常规三孔法腹腔镜胆囊切除术的对比研究[J].腹腔镜外科杂志,2016,21(9):692-695.
Clinical Application of Self-made Modified Specimen Bag in Laparoscopic Cholecystectomy
中图分类号: