

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 81-83.DOI: 10.3969/j.issn.1009-976X.2020.01.018
摘要:
复杂尿路感染(UTI)是尿路由于器质性、功能性异常或与留置导尿管/支架相关的感染,通常传统的抗生素疗效欠佳。泌尿系结石并发梗阻性尿路病并不少见,其导致的急性肾盂肾炎(APN)合并梗阻可发展为尿脓毒症,引起严重的脓毒血症,处理相对复杂、棘手[1,2]。目前认为,除了有效的抗生素治疗外,处理梗阻性尿路病的方法是迅速减压肾集合系统,可选择经皮肾造瘘或逆行输尿管插管术[1]。我院2014年7月~2018年5月收治上尿路结石合并尿脓毒血症43例,采用一期经输尿管镜下逆行插管术或经皮肾穿刺造瘘术解除梗阻,二期行微创手术处理结石等处理,现报道如下。
回顾2014年7月至2018年5月我院确诊收治的43例上尿路结石合并尿脓毒血症患者,均以急性肾区疼痛或慢性疼痛急性加重伴寒战、发热为主要症状,心率加快(98~127 bpm)并血压下降(58~72/30~55 mmHg)12例。患者中,单纯输尿管结石28例(左侧12例,右侧10例,双侧6例),输尿管结石合并肾结石15例(其中合并双肾结石10例),输尿管结石大小约9 mm×6 mm~32 mm×28 mm。所有患者均经超声、腹部平片(KUB)、静脉肾盂造影(IVU)、CT等确诊,B超和CT平扫提示均有患侧肾积水,CT平扫提示肾积水CT值为0~26 H。尿细菌培养阳性32例:大肠埃希菌20例,肺炎克雷伯菌6例,铜绿假单胞菌4例,粪肠球菌2例,其中27例为多重耐药菌;43例患者无死亡。患者一般资料见表1。
表1 43例脓毒血症临床一般资料
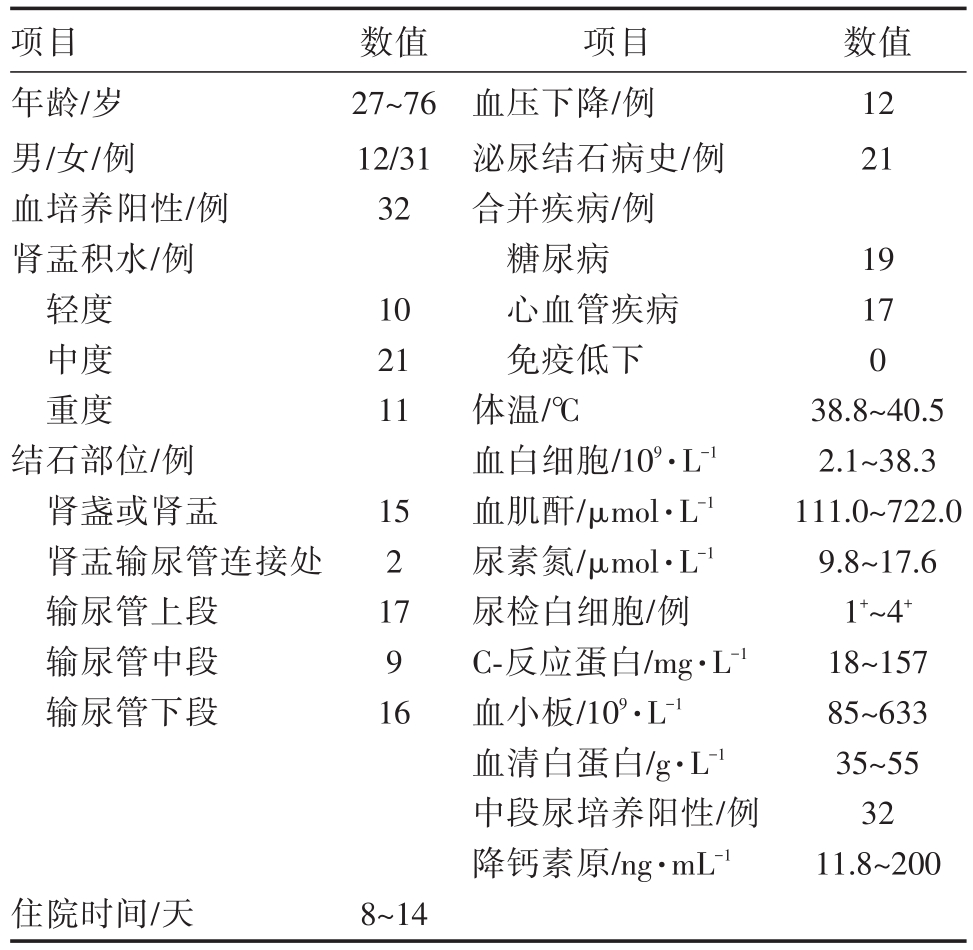
项目年龄/岁男/女/例血培养阳性/例肾盂积水/例轻度中度重度结石部位/例肾盏或肾盂肾盂输尿管连接处输尿管上段输尿管中段输尿管下段数值27~76 12/31 32数值12 21 10 21 11 15 2 17 9 16项目血压下降/例泌尿结石病史/例合并疾病/例糖尿病心血管疾病免疫低下体温/℃血白细胞/109·L-1血肌酐/μmol·L-1尿素氮/μmol·L-1尿检白细胞/例C-反应蛋白/mg·L-1血小板/109·L-1血清白蛋白/g·L-1中段尿培养阳性/例降钙素原/ng·mL-1 19 17 0 38.8~40.5 2.1~38.3 111.0~722.0 9.8~17.6 1+~4+18~157 85~633 35~55 32 11.8~200住院时间/天8~14
患者经确诊后,立即给予广谱抗生素(哌拉西林钠他唑巴坦钠/舒巴坦钠、美罗培南、亚胺培南西司他丁钠等)抗感染、补液、维持酸碱平衡、营养支持、保护细胞膜等治疗,待血培养、尿培养结果回报后,再根据药敏试验结果选用敏感抗生素治疗,合并休克者积极抗休克治疗,休克较难纠正时给予血管活性药物(如去甲肾上腺素、多巴胺、多巴酚丁胺等)治疗。对于积极抗感染等治疗后,病情逐渐稳定的患者给予行经输尿管镜下逆行插管术,术中输尿管进镜至输尿管结石下端,将斑马导丝沿结石旁边插入肾内,沿斑马导丝留置F6双J管一条;对于病情难以控制或经输尿管镜下逆行插管失败的患者,予行B超引导下经皮肾穿刺造瘘术,留置F16肾造瘘管一根。经以上治疗后,患者感染控制、病情稳定后出院,出院1月后再次住院,二期行腔内微创碎石手术治疗结石,其中输尿管镜碎石术(硬镜)28例,输尿管软镜碎石术7例,经皮肾镜碎石术8例,术后输尿管内常规留置F6双J管2~3周,行经皮肾镜碎石术后再留置肾造瘘管3~5日。经以上手术治疗后,术后复查B超、KUB或CT,若见较大结石残留,则予行体外冲击波碎石术治疗。术后3个月复查B超、KUB、或CT、肾功能等。
本组患者中29例患者一期成功行经输尿管镜下逆行插管术,术中留置F6双J管一条,其中单侧结石23例,双侧结石6例,双侧输尿管结石患者双侧输尿管均能一期行逆行插管。行经输尿管镜下逆行插管术失败的6例患者及不宜行逆行插管术的8例患者行B超引导下经皮肾穿刺造瘘术,术中留置F16造瘘管一根。29例逆行插管术后20例及所有经皮肾穿刺造瘘术患者术后有暂时性肉眼血尿,32例有轻度腰部疼痛不适,无输尿管穿孔或断裂、严重出血、肾周血肿、误伤胸膜或腹腔脏器等并发症,43例患者均无感染加重、病情反复。经治疗后,病情稳定,复查血常规白细胞正常、PCT正常、体温正常后出院。出院1月后再次住院,二期行腔内微创碎石手术,碎石成功41例,碎石率95.35%(41/43),2例患者术后行体外冲击波碎石治疗,3个月后复查,42例患者结石排净,结石排净率为97.67%(42/43),肾功能及肾积水程度明显改善。其中肾功能恢复正常39例,4例患者肾功能轻度不全,但血肌酐、尿素氮均较前明显下降;复查B超或CT提示肾积水明显好转,43例患者在整个治疗过程中均未出现严重并发症。
尿脓毒血症的常见原因是尿路梗阻性疾病,如尿路结石、狭窄和肿瘤,本组43例患者均合并输尿管结石梗阻。输尿管结石造成尿路梗阻的同时作为异物能促进尿路感染的发生,尿路感染可以加速结石的增长,两者形成恶性循环。泌尿系结石常合并有尿路感染,结石本身是异物存在于泌尿系中易导致感染发生,而当结石导致梗阻后,引起肾内积水,导致肾内尿液淤积,形成细菌生长的良好环境,随着肾内压力的逐渐增加、细菌感染逐渐加重后,细菌及毒素进入血液,从而逐渐引起全身中毒症状。除泌尿系结石梗阻外,高龄、女性、基础疾病(糖尿病、免疫抑制、截瘫、肾先天畸形)、既往同侧结石手术史等亦为尿脓毒血症的易感因素。
尿脓毒症的严重程度主要取决于宿主反应和局部因素。老年患者和糖尿病和/或免疫抑制患者,如皮质类固醇或免疫抑制剂患者、移植受者和艾滋病患者,表现出宿主防御能力降低[3]。此外,局部因素,如尿路结石、梗阻性尿路病、先天性尿路病、神经源性膀胱疾病和内镜手术,都会影响疾病的严重程度[4]。一些研究证实,细菌性急性肾盂炎症肾炎患者出现尿路梗阻与感染性休克发生的危险因素有关[5,6]。输尿管支架或经皮肾造口术、上尿路梗阻性尿路疾病合并感染时,没有进行有效减压可导致尿脓毒症明显增加(OR 2.6,95%CI 1.9~3.7)[7]。Yo-shimura等报告显示年龄、性别和一般情况差的上尿路结石患者是进行紧急引流的危险因素[8]。另一项研究也显示,年龄和高C-反应蛋白水平是决定上尿路结石引起肾绞痛患者紧急引流的有用参数[9]。
血小板计数和血清白蛋白水平的降低可能是阻塞性呼吸暂停综合征患者感染性休克发生的预测因素[10]。血小板和中性粒细胞在尿脓毒症中起积极作用,它们共同参与炎症反应。中性粒细胞与血小板相互作用介导这一炎症反应的机制,例如在脓毒症模型小鼠和脓毒症患者的肝脏和肺中存在大量血小板[11],这反映血小板在肝和肺中的积聚可能与败血症中血小板的减少有关。另外,血清白蛋白在炎症反应中会降低,这可能是多种因素的结果包括蛋白质分解代谢增加和肝合成减少[12],并且由于炎症过程中血管通透性增加而导致蛋白质血管外丢失。在临床感染的发热患者中,低水平的血清白蛋白是单变量分析中休克发展的预测因素之一[13]。PCT作为炎性反应指标,能提示感染原因、判断病情严重程度和估计预后[14]。近年来,降钙素原(PCT)被用于评估脓毒血症患者的指标,作为炎性反应指标,PCT能提示感染原因、判断病情严重程度和估计预后[14,15]。
尿脓毒血症一经确诊即需积极治疗,Wagen-lehner等[16]认为尿脓毒血症诊断后第一个小时治疗非常关键以防止早期细胞和组织损伤。采取的系列措施旨在迅速引流穿刺减压、早期控制感染病灶、稳定呼吸和心血管功能。早期经输尿管镜下逆行插管或经皮肾穿刺造瘘联合输尿管镜(硬镜或软镜)或经皮肾镜碎石术是治疗上尿路结石合并尿脓毒血症患者的有效方法。
[1] 陈卓,陈刚,金伟,等.上尿路结石合并尿脓毒血症的微创治疗[J].中国微创外科杂志,2015,15(2):118-120.
[2] Wagenlehner FM,Tandogdu Z,Bjerklund Johansen TE.An up-date on classification and management of urosepsis[J].Curr Opin Urol,2017,27(2):133-137.
[3] Geerlings SE.Clinical Presentations and Epidemiology of Uri-nary Tract Infections[J].Microbiol Spectr,2016,4(5).
[4] Wagenlehner FM,Tandogdu Z,Bjerklund Johansen TE.An up-date on classification and management of urosepsis[J].Curr Opin Urol,2017,27(2):133-137.
[5] Lee JH,Lee YM,Cho JH.Risk factors of septic shock in bacte-remic acute pyelonephritis patients admitted to ER[J].J Infect Chemother,2012,18(1):130-133.
[6] Kalra OP,Raizada A.Approach to a patient with urosepsis[J].J Glob Infect Dis,2009,1(1):57-63.
[7] Borofsky MS,Walter D,Shah O,et al.Surgical decompression is lifesaving for patients with sepsis and ureteral calculi[J].J Urol,2013,189(3):946-951.
[8] Yoshimura K,Utsunomiya N,Ichioka K,et al.Emergency drainage for urosepsis associated with upper urinary tract calculi[J].J Urol,173(2):458-462.
[9] Angulo JC,Gaspar MJ,Rodriguez N,et al.The value of C-reac-tive protein determination in patients with renal colic to decide urgent urinary diversion[J].Urology,2010,76(2):301-306.
[10] Tambo M,Okegawa T,Shishido T,et al.Predictors of septic shock in obstructive acute pyelonephritis[J].World J Urol,2014,32(3):803-811.
[11] Andonegui G,Kerfoot SM,Mcnagny K,et al.Platelets express functional Toll-like receptor 4[J].Blood,2005,106:2417-2423.
[12] Ruot B,Breuille D,Rambourdin F,et al.Synthesis rate of plas-ma albumin is a good indicator of liver albumin synthesis in sep-sis[J].Am J Physiol Endocrinol Metab,2005,279(2):E244-E251.
[13] Bossink AW,Groeneveld AB,Koffeman GI,Becker A.Predic-tion of shock in febrile medical patients with a clinical infection[J].Crit Care Med,2001,29(1):25-31.
[14] Sugimoto K,Adomi S,Koike H,Esa A.Procalcitonin as an in-dicator of urosepsis[J].Res Rep Urol,2013,5(1):77-80.
[15] Dreger NM,Degener S,Ahmad-Nejad P,et al.Urosepsis—Eti-ology,Diagnosis,and Treatment[J].Dtsch Arztebl Int,2015,112(49):837-847.
[16] Wagenlehner FM,Lichtenstern C,Weigand MA,Weidner W.Urosepsis and treatment[J].Urologe A,2010,49(5):618-622.
The treatment for upper urinary stones complicated with urosepsis
中图分类号: