

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 12-15.DOI: 10.3969/j.issn.1009-976X.2020.01.003
摘要:
随着腹腔镜技术的改进和手术经验的增加,腹腔镜胆囊切除术(LC)已成为急性胆囊炎(AC)的标准治疗方法。然而,在一些临床情况如胆囊及周围的局部炎症或全身麻醉的高风险下,选择LC、保守治疗还是进行置管引流有时成为外科医生的难题,尤其对于可能危及生命的老年AC患者[1]。经皮经肝胆囊引流术(PTGBD)是一种能够改善AC急性炎症状态的简单易行的手术方法[2,3]。根据东京指南对AC的治疗,PTGBD可以选择性地应用于中重度AC患者[4]。但对于老年中度以上AC患者究竟是首先行胆囊穿刺引流还是采用急诊LC尚未有明确共识,目前采取何种方案主要取决于医生的个人偏好和经验[5,6]。本研究通过比较这两种方案在老年中度AC的应用价值,以期为老年中度AC的治疗等提供依据。
研究对象均签署知情同意书。95例研究对象来自2016年1月至2019年6月湛江中心人民医院肝胆外科收治的老年中度AC患者。入组标准:①中度AC的诊断符合东京指南2013版的中度AC诊断标准[7];②患者年龄≥60岁。排除标准:①患者同时伴有胆总管结石、腹水或弥漫性腹膜炎;②两位副高以上的肝胆外科医师的术前临床评估结果均认为PTGD是唯一选择。通过详细介绍急诊LC、PTGD联合择期LC的治疗方案及各自优缺点后,根据患者的病情、意愿及经济情况等将患者分为PTGBD+LC组(35例)和LC组(60例)。两组的一般情况差异没有统计学意义(P>0.05)。见表1。
表1 两组一般情况比较
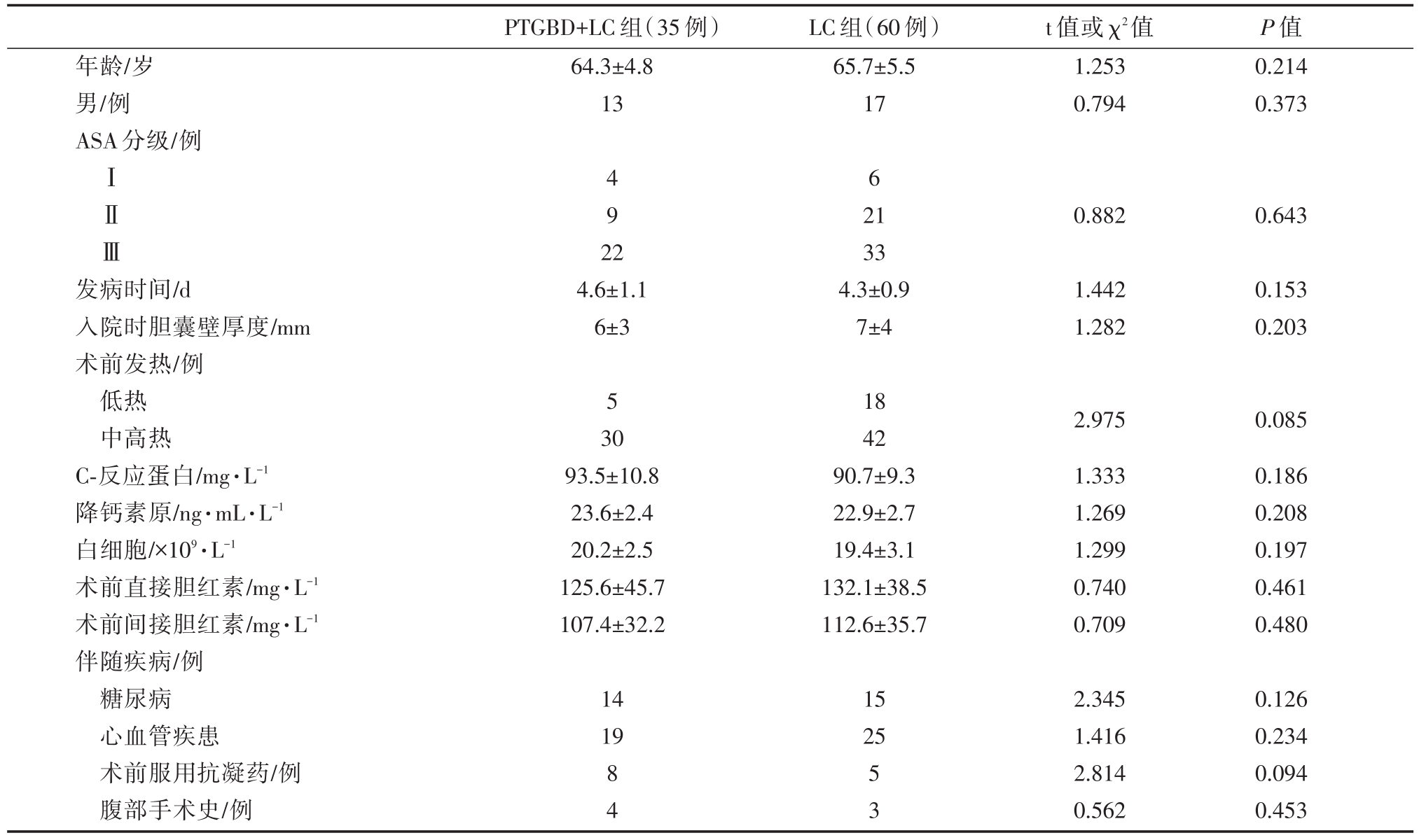
年龄/岁男/例ASA分级/例PTGBD+LC组(35例)64.3±4.8 13 LC组(60例)65.7±5.5 17 t值或χ2值1.253 0.794 P值0.214 0.373ⅠⅡⅢ4 9 2 2 6 0.8820.643发病时间/d入院时胆囊壁厚度/mm术前发热/例低热中高热C-反应蛋白/mg·L-1降钙素原/ng·mL·L-1白细胞/×109·L-1术前直接胆红素/mg·L-1术前间接胆红素/mg·L-1伴随疾病/例糖尿病心血管疾患术前服用抗凝药/例腹部手术史/例4.6±1.1 6±3 21 33 4.3±0.9 7±4 1.442 1.282 0.153 0.203 5 30 93.5±10.8 23.6±2.4 20.2±2.5 125.6±45.7 107.4±32.2 18 42 90.7±9.3 22.9±2.7 19.4±3.1 132.1±38.5 112.6±35.7 2.975 1.333 1.269 1.299 0.740 0.709 0.085 0.186 0.208 0.197 0.461 0.480 14 19 15 25 8 4 5 3 2.345 1.416 2.814 0.562 0.126 0.234 0.094 0.453
LC组采用急诊LC:患者完善必要检查后,依据患者的病情情况行三孔LC。切除胆囊时,先将胆囊动脉、胆囊管与胆囊壁粘连组织分离,然后采用顺逆结合的方法切除胆囊,手术后常规放置腹腔引流管。若术中出现胆囊床和胆囊分离难度大、胆囊三角黏连严重、腹腔内出血难以控制、肠道或胆管损伤等情况,则中转开腹。
PTGBD+LC组采用PTGD联合择期LC。患者先行PTGD(二步法穿刺):患者完善必要检查后,局部浸润麻醉,在B超引导下取右侧腋前线第7至9肋间定位穿刺点,避开肝内血管和胆管,肋角进针,经过2~4 cm肝组织,在胆囊床中、外1/3处穿入胆囊,抽出胆汁。采用超声造影确认穿刺位置正确后,沿穿刺外套管跟入导丝至胆囊内成袢,撤出穿刺外套管,沿导丝跟入引流管,于胆囊内成袢,随后抽取胆汁送检做细菌培养及药物敏感性检测。行PTGD后,根据患者的病情择期行LC。LC与LC组方法相同。
比较两组LC围手术期的评价指标(中转开腹、术中失血量、手术时间、LC后引流时间、LC后住院时间、总住院时间)。采用间接免疫荧光法和免疫速率散射比浊法分别检测两组LC前和LC后第1 d的细胞免疫功能(CD3、CD4、CD8和CD4/CD8)和体液免疫功能(IgA、IgG和IgM)。统计两组并发症。
统计软件为SPSS 24.0。计量资料采用均数±标准差(x±s)表示,采用t检验分析数据。计数资料采用频数和百分率表示,采用Pearsonχ2检验、Yatesχ2检验或确切概率法分析数据。以P<0.05认为差异有统计学意义。
PTGBD+LC组和LC组中转开腹的构成比为5.7%(2例)和25.0%(15例),两者差异有统计学意义(χ2值=4.388,P=0.036)。PTGBD+LC组行PTG-BD到行LC的时间是75.2±5.7 d,引流后抗生素使用时间是5.2±0.9 d。与LC组相比,PTGBD+LC组的LC中失血量明显少;手术时间、LC后引流时间和LC后住院时间明显短,总住院时间明显长(P<0.01)。见表2。
表2 两组LC围手术期的评价指标比较(x±s)
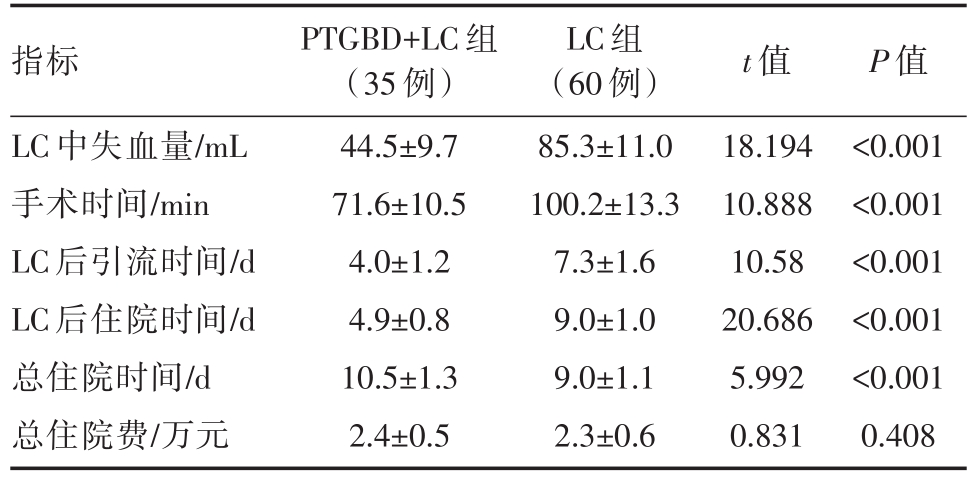
指标LC中失血量/mL手术时间/min LC后引流时间/d LC后住院时间/d总住院时间/d总住院费/万元PTGBD+LC组(35例)44.5±9.7 71.6±10.5 4.0±1.2 4.9±0.8 10.5±1.3 2.4±0.5 LC组(60例)85.3±11.0 100.2±13.3 7.3±1.6 9.0±1.0 9.0±1.1 2.3±0.6 t值18.194 10.888 10.58 20.686 5.992 0.831 P值<0.001<0.001<0.001<0.001<0.001 0.408
PTGBD+LC组和LC组术前的IgA、IgG、IgM、CD3+、CD4+和CD4+/CD8+值均明显高于术后(P<0.05)。PTGBD+LC组术后的IgA、IgG、IgM、CD3+、CD4+和CD4+/CD8+值均明显高于LC组(P<0.05)。见表3。
PTGBD+LC组的并发症总发生率明显低于LC组(P<0.05)。见表4。
表3 两组术前后的细胞免疫与体液免疫指标比较(x±s)

注:与LC组相同时间比较:aP<0.05
PTGBD+LC组(35例)LC组(60)IgA/g·L-1 IgG/g·L-1 IgM/g·L-1 CD3+/%CD4+/%CD8+/%CD4+/CD8+术前3.0±0.6 12.1±3.0 1.8±0.6 65.6±4.4 34.2±4.3 27.1±4.7 1.6±0.4术后2.6±0.5a 10.7±2.8a 1.5±0.5a 63.3±4.8a 32.0±3.9a 25.7±5.0 1.3±0.5a t值3.030 2.018 2.272 2.090 2.242 1.207 2.772 P值0.004 0.048 0.026 0.040 0.028 0.232 0.007术前2.9±0.7 11.5±2.6 1.7±0.7 64.4±5.2 33.7±3.5 26.9±4.5 1.5±0.5术后2.3±0.6 9.4±2.1 1.2±0.6 60.5±4.6 29.4±4.0 26.4±5.2 1.0±0.4 t值5.041 4.867 4.201 4.351 6.267 0.563 6.049 P值<0.001<0.001<0.001<0.001<0.001 0.574<0.001
表4 两组的并发症比较[n(%)]
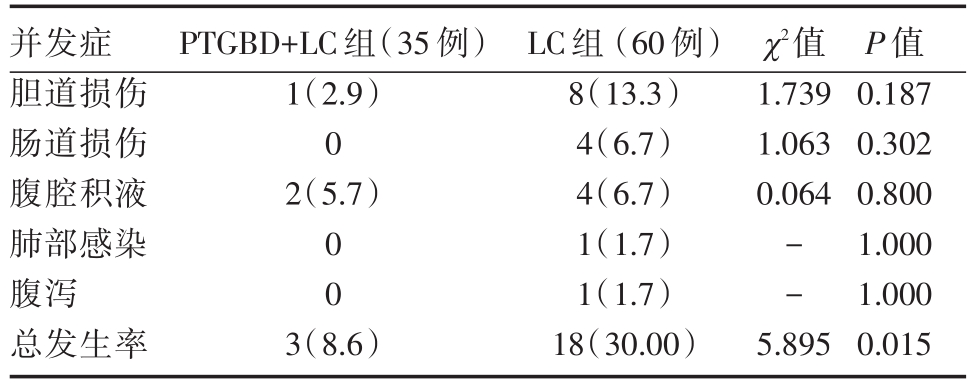
并发症胆道损伤肠道损伤腹腔积液肺部感染腹泻总发生率PTGBD+LC组(35例)1(2.9)0 2(5.7)χ2值1.739 1.063 0.064 0 0--3(8.6)LC组(60例)8(13.3)4(6.7)4(6.7)1(1.7)1(1.7)18(30.00)5.895 P值0.187 0.302 0.800 1.000 1.000 0.015
近年来,随着介入超声微创技术不断在临床上推广应用,超声引导下PTGD,也已成为治疗AC的有效手段[8]。老年AC患者由于器官功能衰退和免疫功能降低,而AC具有发展快的特点,因此发生胆囊穿孔和坏疽的可能性较高[7]。与LC组相比,PTGBD+LC组中转开腹的构成比明显低,LC中失血量明显少,手术时间明显短,提示PTGD联合择期LC可降低LC的难度和风险,提高LC的治疗效果,分析原因可能如下:AC患者经PTGD引流后,胆囊迅速减压,24~72 h能迅速减轻胆囊和胆管系统的压力,缓解症状,控制感染,从而使胆囊体积明显减小,胆囊壁出血、黏膜坏死、周围组织的包裹程度等均显著减轻,出血量明显减少,术野也明显清晰,进而有利于胆囊的分离及胆囊三角的处理,因此LC的难度和风险也随之降低,LC的治疗效果也得到提高[9,10]。与LC组相比,PTGBD+LC组的LC后引流时间和LC后住院时间明显短,提示PTGD联合择期LC可加快老年中度AC患者的术后恢复。分析原因可能如下:①PTGD使术野增大和更加清晰,手术难度下降,可使择期LC的创伤明显轻于急诊LC[11],因此患者恢复较快;②患者的恢复速度与AC的病情有一定关联,PTGD可减轻AC引起的毒血症等,同时必要时可胆囊内注入抗菌药物进行冲洗,从而使AC的病情在行LC之前得到明显改善[12];③PTGD能明显降低老年中度AC中转开腹的发生率[13]。PTGBD+LC组的总住院时间虽然明显长于LC组,但总住院费并不明显增加,提示PTGD联合择期LC并不增加患者的负担。值得注意的是,PTGBD+LC方案也有缺点,例如行PTGBD到行LC的时间需要75 min左右,引流后还需要使用约5天的抗生素。因此,临床医务工作者在选择方案的时候,应根据患者的情况进行个体化处理。
PTGBD+LC组和LC组术前的IgA、IgG、IgM、CD3+、CD4+和CD4+/CD8+值均明显高于术后,提示两种方案对老年中度AC患者的术后免疫球蛋白含量及T淋巴细胞亚群均明显影响,这个结果符合文献报道[14]。PTGBD+LC组术后的IgA、IgG、IgM、CD3+、CD4+和CD4+/CD8+值均明显高于LC组,提示PTGD联合择期LC对细胞免疫和体液免疫的影响比急诊LC明显小,更有利于老年中度AC患者术后恢复,其原因可能如下:机体免疫抑制程度与手术创伤的程度密切相关[15],而PTGBD+LC组的手术创伤相对较轻。其他地区也有类似的报道。
急诊LC具有较高并发症率,如何降低急诊LC的并发症的发生率成为临床研究热点。PTG-BD+LC组的术后并发症总发生率低于LC组,提示PTGD联合择期LC有利于降低老年中度AC患者术后并发症。对于急诊老年中度AC患者,往往由于病情需要导致术前准备不够充分,且由于AC的炎症反应和患者的应激性反应等进一步加重患者的生理功能紊乱,导致并发症的发生率增高。
综上所述,PTGD联合择期LC可明显降低LC的难度和风险,提高LC的效果,加快老年中度AC患者的术后恢复,减轻免疫功能损伤和降低并发症发生率。
[1] Wiggins T,Markar SR,Mackenzie H,et al.Evolution in the management of acute cholecystitis in the elderly:population-based cohort study[J].Surg Endosc,2018,32(10):4078-4086.
[2] 邝乃乐,伍隽华,许洁娜,等.彩超引导下经皮经肝胆囊穿刺置管引流治疗41例高危人群急性胆囊炎[J].岭南现代临床外科,2017,17(6):674-677.
[3] 李驰,吴刚.超声引导下经皮经肝胆囊穿刺置管引流术治疗老年急性结石性胆囊炎的疗效[J].中国老年学杂志,2016,36(04):891-892.
[4] Miura F,Takada T,Strasberg SM,et al.TG13 flowchart for the management of acute cholangitis and cholecystitis[J].J Hepato-biliary PancreatSci,2013,20(1):47-54.
[5] Jung WH,Park DE.Timing of Cholecystectomy after Percutane-ous Cholecystostomy for Acute Cholecystitis[J].Korean J Gas-troenterol,2015,66(4):209-214.
[6] 许承,郑跃,王军,等.PTGD术后择期LC对GradeⅡ急性胆囊炎患者手术效果的影响[J].实用医学杂志,2018,34(07):1119-1122.
[7] Yokoe M,Hata J,Takada T,et al.Tokyo Guidelines 2018:di-agnostic criteria and severity grading of acute cholecystitis(with videos)[J].J Hepatobiliary Pancreat Sci,2018,25(1):41-54.
[8] Tian H,Xia M,Zhang S,et al.Acute calculouscholecystitis as-sociated with hepatic artery pseudoaneurysm after percutaneous transhepatic gallbladder drainage in a diabetic patient[J].Chin Med J(Engl),2014,127(17):3192-3194.
[9] 邱明,吴向未,杨宏强,等.急性胆囊炎经皮经肝胆囊穿刺引流术后手术时机的选择[J].实用医学杂志,2014,30(18):2911-2914.
[10] 柯昌伟,吴硕东,李勇男.中度急性胆囊炎行急诊胆囊切除与经皮经肝胆囊穿刺引流术加择期胆囊切除的疗效对比分析[J].中华医学杂志,2018,98(10):768-772.
[11] Baron TH,DeSimio TM.New ex-vivo porcine model for endo-scopic ultrasound-guided training in transmural puncture and drainage of pancreatic cysts and fluid collections(with videos)[J].Endosc Ultrasound,2015,4(1):34-39.
[12] 黄美泰,陈焕伟.经皮肝胆囊穿刺引流联合腹腔镜胆囊切除治疗急性化脓性胆囊炎[J].岭南现代临床外科,2013,13(3):208-2180.
[13] Rajcok M,Bak V,Danihel L,et al.Early versus delayed lapa-roscopic cholecystectomy in treatment of acute cholecystitis[J].Bratisl Lek Listy,2016,117(6):328-331.
[14] 李永贵.经皮经肝胆囊穿刺引流术联合腹腔镜胆囊切除术治疗急性危重胆囊炎的短期疗效及对患者免疫功能的影响[J].中国老年学杂志,2017,37(23):5898-5900.
[15] 张伟,于在诚.食管癌患者不同术式围手术期细胞免疫与体液免疫的监测分析[J].广东医学,2015,36(10):1545-1547.
Percutaneous transhepatic gallbladder drainage combined with elective laparoscopic cholecystec-tomy in elderly patients with moderate acute cholecystitis
中图分类号: