

岭南现代临床外科 ›› 2020, Vol. 20 ›› Issue (01): 8-11.DOI: 10.3969/j.issn.1009-976X.2020.01.002
摘要:
全系膜切除(total mesorectal excicion,TME)的标准手术方式提出和直肠双吻合技术(double sta-pling technique,DST)的广泛应用,使得中低位直肠残端吻合位置可以更低。由于括约肌保留率的提高,对低位前切除术(low anterior resection,LAR)术后吻合口漏(anastomotic Leakage,AL)的关注程度不断提高,降低吻合口漏也是中低位直肠癌保肛术后康复的关键,但目前尚没有找到预防AL的理想方法。已经报道了几种AL的危险因素,但尚不清楚预防AL的原因和理想方法。近些年来的报道显示,吻合口部的压力降低对于预防AL非常重要,而使用经肛门引流管(TDT)可以降低直肠压力[1-6]。为此,我院采用盆底腹膜重建联合肛管引流来预防直肠癌术后吻合口漏的发生,其临床疗效报道如下。
回顾性分析2013年1月至2017年12月在我院就诊的137例中低位直肠癌患者手术资料,男性 74例,女性 63例;年龄 35~81岁,(56.8±8.3)岁。所有患者均行肠镜检查,病理证实均为直肠癌。并行CT和或MIR检查,明确肿瘤有无侵犯临近脏器及远处转移。术前检查提示:肿瘤均为中下段(肿瘤距肛齿状线4~10 cm),平均(5.38±1.21)cm肿瘤直径2.1~7.3 cm,平均(5.49±0.64)cm,其中4例瘤体较大患者采取四次mFOLFOX6方案的新辅助化疗,未行放疗,瘤体较前缩小后手术。所有患者按常规围手术期行术前准备,无明显手术禁忌症后均行腹腔镜中低位直肠癌前切除术,2例加行腹腔镜肝左叶转移瘤一期切除术。术中行盆底腹膜重建并经腹膜外置入双套管至骶前吻合口旁,同时在术者腔镜指引下经肛置入肛管引流管,术后根据引流液性状,待患者肛门排气/排便恢复后1~4天拔除肛管,平均(2.47±0.45)天。
患者全身麻醉,取改良截石位,常规消毒铺巾。严格遵循TME手术的原则,在腹腔镜下采用直肠后方入路、两侧包抄、前方会师的路径分离直肠周围间隙,锐性分离直肠后间隙至直肠骶骨筋膜,视肿瘤病变位置的高低可继续向尾侧分离至肛提肌上间隙,游离直肠及系膜,于肿瘤远端3~5 cm处裸化肠管,使用腔镜下直线型切割闭合器离断直肠,经肛门用碘伏冲洗直肠下段,注入30 mL碘伏观察残端有无渗漏。29-33号管状吻合器自肛门进入与近端结肠行端端吻合。吻合后盆腔内注水,并经肛门注入空气,无气泡,确定吻合口无漏(图1)。经腹膜外放置双套管引流管于骶前直肠吻合口旁,由下腹引出,用丝线将引流管固定于腹壁(图3)。同时,在腹腔镜直视,术者的指引下,在直肠肠腔内放置留有侧孔的22-28号橡胶引流管,其上端超过吻合口(5~8 cm),肛旁皮肤固定,术后接引流袋引流。气腹压降到8 mmHg(1 mmHg=0.133 kPa),用不可吸收的3-0普理灵缝线从膀胱直肠陷窝或子宫直肠陷窝开始连续缝合重建盆底腹膜(图2、4、5)。
腹腔镜直肠癌切除术后吻合口漏的治疗关键在于早发现早治疗,吻合口漏多发生在术后2~7天,术后吻合口漏的早期表现为持续中度到高度发热、骶尾部、会阴部疼痛不适及引流夜性状改变。由于盆底腹膜重建,早期漏较局限,盆腔引流管引出浑浊脓性及粪水样液体较易观察,引流量在几十到几百毫升不等,但早期出现腹痛、腹胀、弥漫性腹膜炎情况较少。早期结合临床表现、盆腔引流液的量和性质的的改变,一般不难发现,还可以通过B超、CT检查消化道造影等进一步确诊并明确吻合口漏的部位及大小。
137例手术均顺利,无中转开腹,无一例死亡,术中出血量约35~120 mL;术后病理结果全部符合直肠癌,两端切缘病理均阴性。术后吻合口漏发生9例,男性6,女性3例,吻合口漏发生率为6.57%,1例男性术后第7天出现吻合口漏,因感染性腹膜炎并感染性休克再次行回肠末端造口,8例经充分引流、经双套管盆腔冲洗、肠外营养、维持水电解质酸碱平衡和加强抗感染等保守治疗后痊愈。出院后随访3~12个月,平均(7.7±3.3)月,术后复查肠镜、全腹CT等,均未见吻合口狭窄、肿瘤复发及远处转移。

图1 盆底注水测漏

图2 倒刺线连续缝合重建盆底腹膜

图3 经腹膜外建立骶前吻合口旁引流管通道
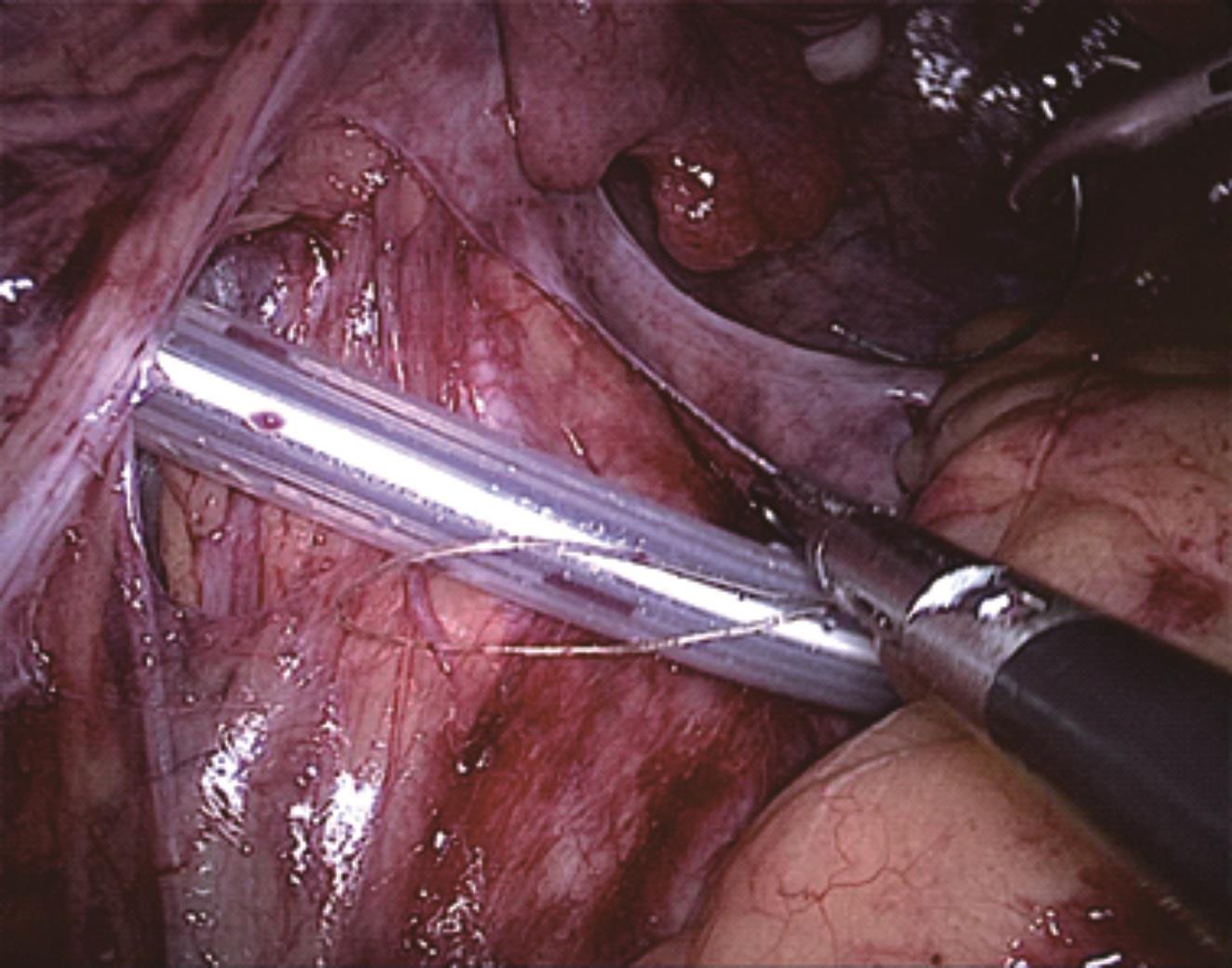
图4 经腹膜外置入引流管并关闭盆底腹膜
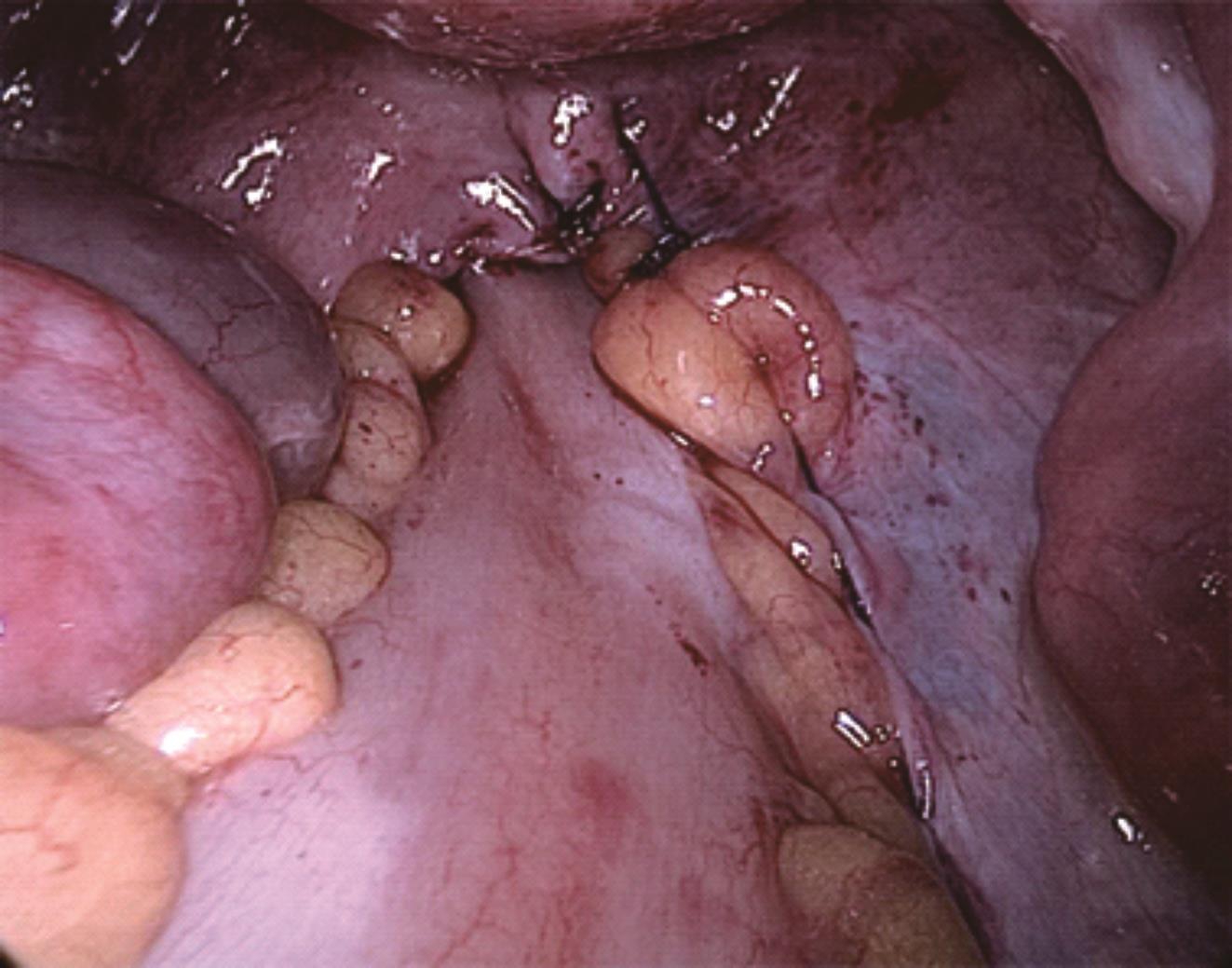
图5 术后盆底腹膜重建效果
近年来,腹腔镜微创技术的日益成熟,TME手术方式和DST技术在直肠癌前切除手术的有效应用,使得直肠癌术后生存率及保肛率取得显著的提高,但吻合口漏的发生率并没有明显改善。吻合口漏是直肠癌术后严重的并发症,吻合口漏的发生不仅增加了术后感染的风险、住院时间的延长、后续治疗的延误、医疗费用的增加等,甚至增加围手术期病死率。相关文献报道,直肠癌术后吻合口漏的发生率为1%~24%,加上无症状的漏,可高达50%[8]。Katsuno等[9]对1014例中低位直肠癌行TME手术患者进行分析,结果显示腹腔镜术后吻合口漏发生率高达15.3%。为降低吻合口漏的概率,国外甚至常规行预防性造口术[10]。如何有效预防直肠癌前切除术后吻合口漏的发生,是我们胃肠道医生共同面临的难题。
吻合口漏的发生与很多因素有关,包括个体相关因素、疾病相关因素、手术相关因素及术后相关因素[11,12]。个体因素有:性别、肥胖、营养状况、美国麻醉医师协会(American Society of Anesthesi-ologists,ASA)分级,而III-V级ASA是吻合口漏的独立危险因素[13]。疾病相关因素:肿瘤的位置、肿瘤大小、术前新辅助治疗、疾病合并其他病发症。手术相关因素:腹腔镜手术、吻合口血供、吻合口张力、预防性造口、其他相关术中因素。术后因素:术后肠道梗阻、心肺/肾功能衰竭、切口感染、深静脉血栓形成等[14]。
因此,我研究中心在中低位直肠癌手术中采用常规关闭盆底腹膜并经腹膜外置入盆腔引流管,同时联合经肛置入肛管来预防术后吻合口漏的发生。以往,在开放低位直肠癌前切除术中常规关闭盆底腹膜,而在腹腔镜下重建盆底腹膜难度大、延长手术时间,许多中心基本采取不关闭盆底腹膜的方法,至使吻合口与腹腔相通,仅仅留置盆腔吻合口旁引流管。重建盆底腹膜减少了继发出血和感染的概率[15],也可以减少盆腔脓肿、吻合口漏及继发腹腔感染的概率[16]。同时,腹腔镜直肠癌前切除术由于直肠全系膜切除加淋巴清扫等,手术范围广创面巨大,术后容易发生盆腔渗液。如果引流不畅,则可能导致盆腔感染、腹膜炎等,影响吻合口愈合,是造成术后吻合口漏的重要因素之一。盆底腹膜的关闭并肛管引流使吻合口周围形成相对闭合负压状态,使吻合口与周围盆壁软组织增加黏连接触机会,从而减少吻合口愈合时间。而通畅引流加盆腔冲洗是治疗术后吻合口漏的重要手段。腹膜外置管引流,使引流管位置相固定,可以达到良好的引流效果。
另外,中低位直肠癌前切除术后吻合口位置较低,而术后直肠腔内压力随肠道功能的恢复和肛门括约肌收缩力的恢复而逐渐增加,吻合口越低,肠腔内压力越大,发生吻合口漏的概率就增加。研究表明,距肛缘<5 cm的低位吻合口漏的发生率为11.6%,显著高于高位吻合口漏的发生率[17]。术后肠内容下排至吻合口周围时,受术中扩肛的影响,只有直肠内积聚足够多且达到一定的肠内压时,才能引起排便反射,而这样的肠内压过高则容易增加吻合口漏的风险[18]。目前有些研究中心提倡术后预防性造口,以减轻吻合口周围压力。但有研究表明,预防性造口并不降低吻合口漏的发生率[19]。术后留置肛管引流可以及时引出肠内容物,降低肠腔内压力,减轻吻合口张力,对吻合口漏起到一定程度的预防作用[20,21],从而降低二次手术的风险。
综上所述,随着腹腔镜下中低位直肠癌前切除术的广泛应用,术后吻合口漏的防治也越加得到重视,盆底腹膜重建联合肛管引流在预防中低位直肠癌前切除术后吻合漏中效果明显,操作简便,值得在临床中推广。
[1] Xiao L,Zhang WB,Jiang PC,et al.Can transanal tube place-ment after anterior resection for rectal carcinoma reduce anasto-motic leakage rate? A single-institution prospective random-ized study[J].World J Surg,2011,35(6):1367-1377.
[2] Zhao WT,Hu FL,Li YY,et al.Use of a transanal drainage tube for prevention of anastomotic leakage and bleeding after an-terior resection for rectal cancer[J].World J Surg,2013,37(1):227-232.
[3] Nishigori H,Ito M,Nishizawa Y,et al.Effectiveness of a trans-anal tube for the prevention of anastomotic leakage after rectal cancer surgery[J].World J Surg,2014,38(7):1843-1851.
[4] Lee SY,Kim CH,Kim YJ,Kim HR.Impact of anal decompres-sion on anastomotic leakage after low anterior resection for rec-tal cancer:a propensity score matching analysis[J].Langen-beck's Arch Surg,2015,400(7):791-796.
[5] Kawada K,Takahashi R,Hida K,Sakai Y.Impact of transanal drainage tube on anastomotic leakage after laparoscopic low an-terior resection[J].Int J Colorectal Dis,2018,33(3):337-340.
[6] Hidaka E,Ishida F,Mukai S,et al.Efficacy of transanal tube for prevention of anastomotic leakage following laparoscopic low anterior resection for rectal cancers:a retrospective cohort study in a single institution[J].Surg Endosc,2015,29(4):863-867.
[7] Snijdersa HS,Leersum NJV,Kolfschoten N E,et al.Meta-anal-ysis of the risk for anastomotic leakage,the postoperative mortal-ity caused by leakage in relation to the overall postoperative mor-tality[J].Eur J Surg Oncol,2012,38(11):1013-1019.
[8] Shogan BD,Carlisle EM,Alverdy JC,et al.Do we really know why colorectal anastomoses leak?[J].J Gastrointest Surg,2013,17(9):1698.
[9] Katsuno H,Shiomi A,Ito M,et al.Comparison of symptomatic anastomotic leakage following laparoscopic and open low anteri-or resection for rectal cancer:a propensity score matching analy-sis of 1014 consecutive patients[J].Surg Endosc,2016,30(7):2848-2856.
[10] Huser N,Michalski CM,Schuster T,et al.Systematic Review and Meta-Analysis of the Role of Defunctioning Stoma in Low Rectal Cancer Surgery[J].Ann Surg,2008,248(1):52-56.
[11] 陶凯雄,高金波.直肠癌术后吻合口漏发生的危险因素[J].中华胃肠外科杂志,2018,21(4):384-387.
[12] 周灿,陈武科,何建军,等.国内直肠癌术后吻合口瘘危险因素的Meta分析[J].西安交通大学学报(医学版),2010,31(1):115-121.
[13] Choi HK,Law WL,Ho JW.Leakage after resection and intra-peritoneal anastomosis for colorectal malignancy:analysis of risk factors[J].Dis Colon Rectum,2006,49(11):1719 -1725.
[14] Kang CY,Halabi WJ,Chaudhry OO,et al.Risk factors for anastomotic leakage after anterior resection for rectal cancer[J].JAMA Surg,2013,148(1):65-71.
[15] Rahbari NN,Weitz J,Hohenberger W,et al.Definition and grading of anastomotic leakage following anterior resection of the rectum:a proposal by the International Study Group of Rectal Cancer[J].Surgery,2010,147(3):339-351.
[16] 付正伟,王丽霞,张振宇,等.盆底腹膜重建在3D腹腔镜辅助直肠前切除术中的价值[J].中华腔镜外科杂志(电子版),2018,11(2):94-97.
[17] Pommergaard HC,Gessler B,Burcharth J,et al.Preoperative risk factors for anastomotic leakage after resection for colorectal cancer:a systematic review and meta-analysis[J].Colorectal Dis,2015,16(9):662-671.
[18] 杜晓辉,邢晓伟.机器人直肠癌术后吻合口漏的预防策略[J].中华胃肠外科杂志,2018,21(4):395-398.
[19] Shiomi A,Ito M,Maeda K,et al.Effects of a diverting stoma on symptomatic anastomotic leakage after low anterior resection for rectal cancer:a propensity score matching analysis of 1,014 consecutive patients[J].J Am Coll Surg,2015,220(2):186-194.
[20] Yang CS,Choi GS,Park JS,et al.Rectal tube drainage reduc-es major anastomotic leakage after minimally invasive rectal can-cer surgery[J].Colorectal Dis,2016,18(12):442-445.
[21] Ito T,Obama K,Sato T,et al.Usefulness of transanal tube placement for prevention of anastomotic leakage following lapa-roscopic low anterior resection.[J].Asian J Endosc Surg,2016,10(1):17.
The application of pelvic floor peritoneal reconstruction combined with transanal drainage in prevention of anastomotic leakage after laparoscopic rectal cancer anterior resection
中图分类号: